A mixed-methods study on the implementation of a mobile health application (mHealth app) for stroke caregivers in Malaysia: healthcare providers’ perspective
1. Introduction
Stroke has become a leading cause of preventable disability, and the burden has increased worldwide over the past two decades (1). In 2017, about one in every two Malaysian stroke survivors was discharged with physical disabilities (2) and required aid and extensive care to adjust to their new life. These include performing activities of daily living (ADLs), rehabilitation support, medication care, companionship, and emotional support (3, 4).
The World Health Organization (WHO) Global Observatory for eHealth defined mHealth apps as mobile applications and other wearable devices that collect and monitor users’ medical information (5). Studies have indicated that it enhances the excellence and inclusivity of healthcare; expands access to health-related information, services, and expertise; and fosters improved health-related behaviors (6–8). With limitations in the health system, such as human resources, infrastructure, financial support, and the caregivers themselves (including a lack of social support, logistical issues, and geographic factors), this mHealth intervention seems to bring forth a promising solution in stroke caregiving (9–13).
Numerous non-pharmacological treatment modalities, such as psychoeducational and psychosocial information, and skill-building interventions have been adopted and delivered on various digital platforms (including mobile health applications) to assist and empower stroke caregivers (14–17). A scoping review of seven articles regarding mHealth apps for family caregivers in preventing recurrent stroke revealed that many apps used video education, exercise reminders, access to stroke-related information, and feedback mechanisms (17). The studies were conducted in seven countries, namely the United States, Pakistan, the Netherlands, Korea, India, China, and Sweden, and all studies were conducted to test the feasibility of the apps in question (17). Another review of 47 apps that were available on the Android and/or iOS platforms and tailored to caregivers during stroke patient recovery revealed that such apps contained features that support caregivers’ wellbeing, role adaptation, and engagement in patient management (18). The sources or contents of the apps were derived from Australia, Canada, India, Singapore, Spain, and the United States. However, some of them could not be identified.
Due to the unavailability of an app that is culturally tailored to Malaysia and specific for stroke caregivers, a megaproject was launched in 2019 through a collaboration between Universiti Sains Malaysia and the London School of Hygiene and Tropical Medicine (LSHTM) (19), with the aim of developing an app that can help enhance the caregivers’ ability to handle the physical and psychological requirements of stroke survivors, as well as their own personal needs (19). This project was based on the success of an application known as “Care for Stroke,” a smartphone-enabled intervention for stroke patients that was tested in India and was regarded as acceptable by more than half of stroke survivors and 90% of caregivers (20).
Nevertheless, prior to developing an mHealth app, it is crucial to explore the acceptability of healthcare providers and their expectations of this intervention. The concept of “acceptability” was employed to refer to how users perceive a system prior to its use (21, 22). Healthcare providers who are responsible for providing stroke care and engaging with both patients and caregivers are in a prime position to introduce this mHealth app during their regular duties. The perspective that healthcare providers hold toward this technology could significantly impact the willingness of patients and caregivers to adopt it (23–25). Furthermore, the reasons for low mHealth app usage rates include healthcare providers’ perspectives, acceptability, and over-reliance on traditional face-to-face interventions (25, 26). Overall, this created a need to explore the acceptability of healthcare providers toward adopting digital health interventions prior to app development.
Apart from concerns regarding the suitability and adaptability of the app’s contents to the local context, most studies have applied quantitative methods to assess the acceptability aspect (21, 22, 27, 28). Acceptability should be researched using a variety of methods, combining specific, detailed insights from qualitative research, which is inclined to be based on interpretivism, with generalizable, easily replicable data from quantitative research supported by positivism (27). To bridge these gaps and yield more credible results, this study aimed to present mixed-method research to explore the acceptability of healthcare providers for the implementation of an mHealth app in stroke care. The quantitative component measured mHealth acceptability, while the qualitative component deeply explored the perception and expectations of stroke healthcare providers toward mHealth. The extent to which stroke healthcare providers’ acceptability toward the mHealth app supported or contradicted their perceptions and expectations was observed. It is hoped that the results could provide a piece of holistic evidence by combining inductive and deductive thinking.
2. Methodology
2.1. Study design
The study was conducted based on a pragmatic paradigm, which aims to comprehensively answer the research questions by applying the most effective methods to solve practical issues in the real world, allowing the use of various data sources and knowledge (28). A concurrent mixed-methods design was applied to align with this approach, with quantitative and qualitative data collected simultaneously within the same timeframe (29).
2.2. Study setting and study population
This study was conducted in Malaysia’s northeast coastal regions between 1 June 2021 and 12 November 2021. Our study sample consisted of healthcare providers, such as neurologists, rehabilitation physicians, nurses, occupational therapists (OT), and physiotherapists (PT), from various government health sector facilities, including tertiary hospitals, district hospitals, and primary care facilities. Only the healthcare providers with at least one year of experience managing stroke survivors were included in this study.
To obtain an appropriate sample size for the qualitative component, the principle of saturation was implemented, which meant conducting interviews until no new information or perspective could be obtained (29, 30). Based on a previous study, the required number of participants ranged from 10 to 24 (31–33). To ensure a range of perspectives, experiences, and viewpoints, participants in the interviews were enrolled purposefully using the maximum variation sampling (different professions, ages, sexes, and facility settings) technique (34).
For the quantitative component, sample size estimation was performed using the Krejcie and Morgan formula (35), with the total number of occupational therapists and physiotherapists reported as 279 (36). The total number of physicians, including neurologists, rehabilitation physicians, medical officers, and rehabilitation nurses, based on the staff registry in the respective facilities, was approximately 80. Hence, the minimum sample size required was 186 participants, involving 156 therapists and 30 other stroke healthcare providers.
2.3. Study procedures
2.3.1. Qualitative data collection and sampling
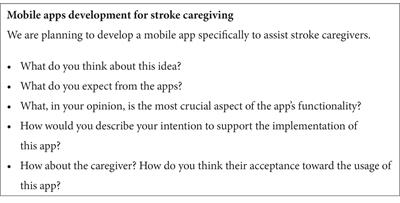
This component employed semi-structured individual interviews with an interview guide as the research instrument (Table 1) (37). Two pilot interviews, which were not included in the sample, were conducted to refine the interview guide and gain deeper insight into the procedure.
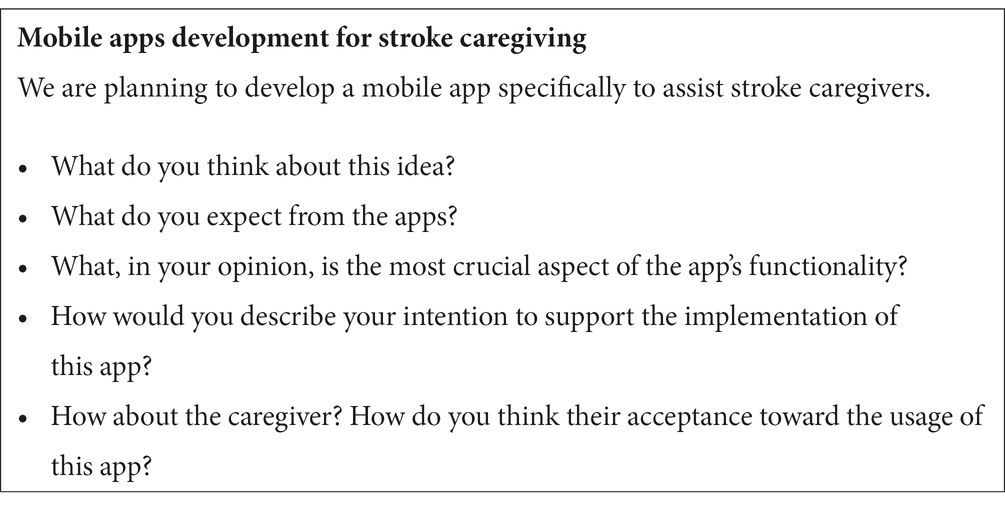
Table 1. Topics for the in-depth interviews.
For participant recruitment, the snowball sampling method was used (38), whereby the names of those eligible and interested in participating in the interview were obtained from the head of the respective profession and contacted by phone. The interviews were planned to be conducted in person, but due to the unforeseeable outbreak of the COVID-19 pandemic and the implementation of associated mitigation measures as well as logistical difficulties related to conducting face-to-face interviews, the interviews were performed using telephone or video conferencing via Webex at the participants’ convenience. Interviews were conducted either in Malay or English language, depending on the participants’ preferences. Digitally recorded interviews were transcribed verbatim in their original languages. Participants were assigned identifying codes to ensure privacy and data management. The audio-recorded interviews and transcribed data were encrypted and stored securely with only the first author accessing them.
To establish trustworthiness, the following four criteria were proposed by Lincoln and Guba: credibility, confirmability, dependability, and transferability (39). The research team ensured credibility by constantly reviewing the results, ensuring sufficient time was allocated for data acquisition, and engaging in research for even longer periods. Confirmability was obtained by recruiting experienced stroke treatment healthcare professionals, and all research features were thoroughly reviewed to meet transferability requirements (34). Member checking was employed to validate the results by discussing the findings with selected participants to guarantee their correctness in reflecting their perspectives and experiences (34). Furthermore, the investigator triangulation method was used to remove researcher bias by comparing preliminary interpretations and findings with the original data (34).
2.3.2. Quantitative data collection and sampling
For this component, to ensure the clarity and comprehension of questionnaires, face validity was conducted before the data collection process, involving 10 healthcare providers, namely 3 physicians, 5 therapists, and 2 nurses. These individuals were excluded from this study. Based on the ratings, the questionnaire had good overall face validity (S-FVI/UA = 0.88; S-FVI/Ave = 0.99). Some questions were rephrased based on expert opinions and their applicability to stroke healthcare providers.
Subsequently, a cross-sectional study was conducted using a structured questionnaire. The questionnaire consisted of 2 sections and 23 questions. The first section contained nine items, organized as follows: (i) sociodemographic profile, including the aspects of sex, age, profession, highest education level, place of work, state, and work experience in stroke management; (ii) self-reported internet skill, in which participants were asked if they could use the Internet for a daily purpose, such as checking and replying to an email, browsing the Internet, and searching for information, which were coded as “very good,” “good,” “average,” “fair,” and “poor”; and (iii) availability and usage of technology at their workplace. The selections for technology usage items were designed based on the technology available in Malaysia: electronic patient records, online self-management or treatment modules, online patient files (via a secure portal), making online appointments, a website for client information (e.g., downloading resources from the Ministry of Health portal), online training, electronic/online screening, eConsult (secure email contact with the client), telemedicine (video calling and remote care), Hospital Information System (HIS), and others. The research team developed sociodemographic and job-related factors based on relevant factors that may impact the acceptability of mHealth as well as information from previous studies (40, 41).
The second section contained the adjusted version of the technology acceptance model (TAM) questionnaire, which measures the intention of healthcare providers to adopt and support mHealth app usage, adapted with the author’s permission (40). The questionnaire was designed based on the core constructs of TAM (42). This 14-item questionnaire assessed perceived usefulness (6 items), perceived ease of use (6 items), and intention to use (2 items). Each item was scored on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree), with 4 as the neutral center of the range.
The convenience sample and snowballing strategy were implemented with the help of each profession’s head and liaison officer to identify eligible participants (38). This cross-sectional, anonymous survey was conducted online using Google Form®, a cloud-based survey tool, and shared through email and WhatsApp® to overcome geographical limitations and restrict physical contact considering the COVID-19 outbreak.
Once all responses were collected, a psychometric evaluation of the questionnaire’s internal structure was performed to ensure its validity and reliability. Internal consistency and factorial structure were examined using exploratory factor analysis (EFA), which showed that the data were normally distributed. The sampling adequacy was excellent, as evidenced by the statistically significant Bartlett’s test and KMO value of 0.953. The 14 items were subjected to a principal component analysis, which revealed an apparent factor structure (Supplementary Table S1). The varimax schedule-rotated component matrix indicated satisfactory loading of all items on their corresponding factors, accounting for 88.88% of the variation in the dependent variable (35.79, 35.02, and 18.07% for factors 1, 2, and 3, respectively). None of the items required deletions in the EFA model.
As for the internal consistency and reliability, Cronbach’s alpha ranged between 0.965 and 0.975. These results indicated that the questionnaire used in this study was valid and reliable for measuring the acceptability of mHealth among healthcare providers.
2.4. Data analyses and integration technique
For the qualitative component, the qualitative data analysis software NVivo® for Windows (QSR International, release 1.5.2, 2021) was used for qualitative data management. All transcribed audio recordings were exported to software and processed using inductive theme analysis (43). The process of data analysis entailed becoming acquainted with the data, creating initial codes, consolidating codes into themes, and assessing, defining, naming, and reporting themes (43). The first, second, and third authors were responsible for the data coding and qualitative data analysis. Any coding disagreements were discussed and settled by consensus within the study team.
Regarding the quantitative component, questionnaires were retrieved from Google Form® and inserted into the IBM SPSS® version 26.0 software for Windows (IBM Corp., Version 26.0, Armonk, NY) for analysis. Descriptive data were reported as frequency (proportion) for categorical data, and mean (standard deviation, SD) was used for numerical data. The Student t-test and Fisher-exact test were used to compare the participants’ characteristics between the qualitative and quantitative components. Meanwhile, to look for possible individual variations in the quantitative component, the Student t-test or one-way ANOVA was applied, depending on the variables. A p-value of less than 0.05 was considered statistically significant.
After conducting the primary data analysis, the research team discussed the possibility of combining the two datasets. A convergent design was employed to explore healthcare providers’ acceptability and expectations concerning mHealth more thoroughly. Given that the quantitative scales and initial qualitative interview questions about acceptability were administered concurrently, this approach allowed for more comprehensive data analysis. A narrative weaving approach was applied to describe and merge the outcomes of the first part by reporting the findings of both components together on a theme-based basis (44). The joint display technique was then utilized to present quantitative and qualitative data together for easy comparison and interpretation (29).
2.5. Ethical considerations
The study was registered and approved by all responsible ethics committees (Malaysia Research Ethics Committee, MREC Ref: KKM/NIHSEC/P20-922), the Human Research Ethics Committee of USM (JEPeM: USM/JEPeM/20010031), and the London School of Hygiene & Tropical Medicine (LSHTM) Research Ethics Committee (LSHTM Ethics Ref: 19079). Regarding the qualitative aspect of the study, participants were given a detailed explanation, both orally and in writing, about the study’s objectives, their voluntary participation, and the secure management of their audio recordings. Following the data collection, all interview transcripts were promptly anonymized. Every participant provided consent to participate in the study and to record their interviews, both verbally and in writing. Compensation of RM 50 was offered to the participants for their time. For the quantitative component, the online survey incorporated the consent form, and individuals who did not provide their consent were unable to proceed to the survey section. Compensation of RM 20 was provided to the participants.
3. Results
3.1. Descriptive summary of respondents’ background information
Table 2 presents the characteristics of participants in both components, whereby both groups were comparable with no significant differences in age, sex, or working experience. For the qualitative component, 12 healthcare providers were interviewed for an average of 30 min. Meanwhile, for the quantitative component, there were a total of 265 healthcare providers who participated in the survey, but 38 responses had to be discarded due to insufficient information. Thus, a total of 227 participants with a mean (SD) age of 34.9 (6.36) years were included in the quantitative analysis. Most participants (n = 173, 76.2%) were women, with half of them working as physiotherapists at hospitals (either tertiary or district), with a mean (SD) working experience in stroke care of 7.0 (4.95) years.
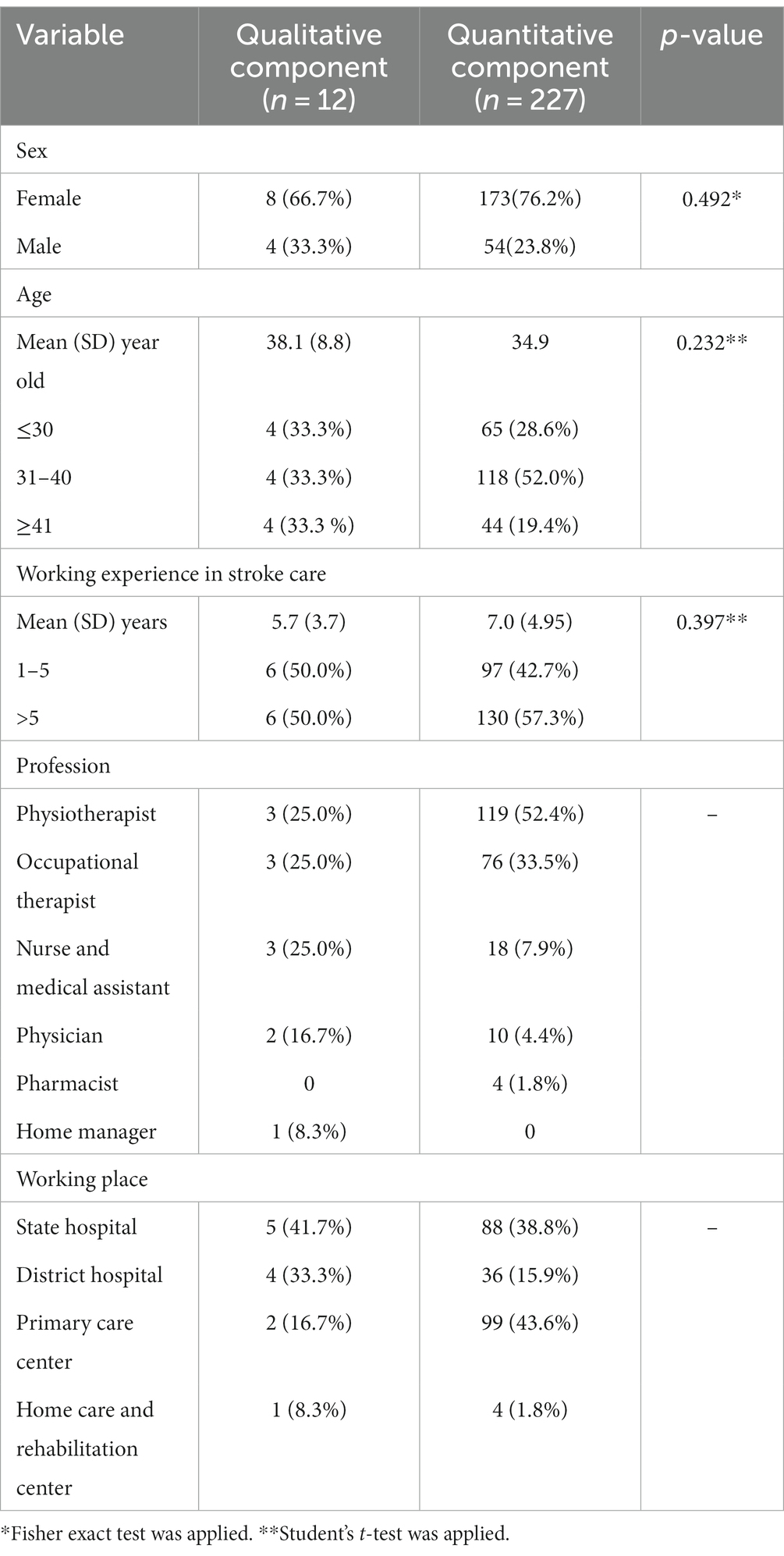
Table 2. Participant characteristics.
Assessment of any potential individual variance in the quantitative component was performed, and Table 3 represents the mean scores for each TAM domain for subgroups of the sample, based on sex, age group, profession, working experience group, working place, and internet skills. The analysis showed no significant differences between all respondent characteristics for domain perceived ease of use. A similar outcome was observed for perceived usefulness except for profession, but further analysis using the Bonferroni-corrected post hoc revealed no significant difference between any groups. With regards to intention to use; profession, working experience, and internet skills were found to influence the intention to use the mhealth app significantly.
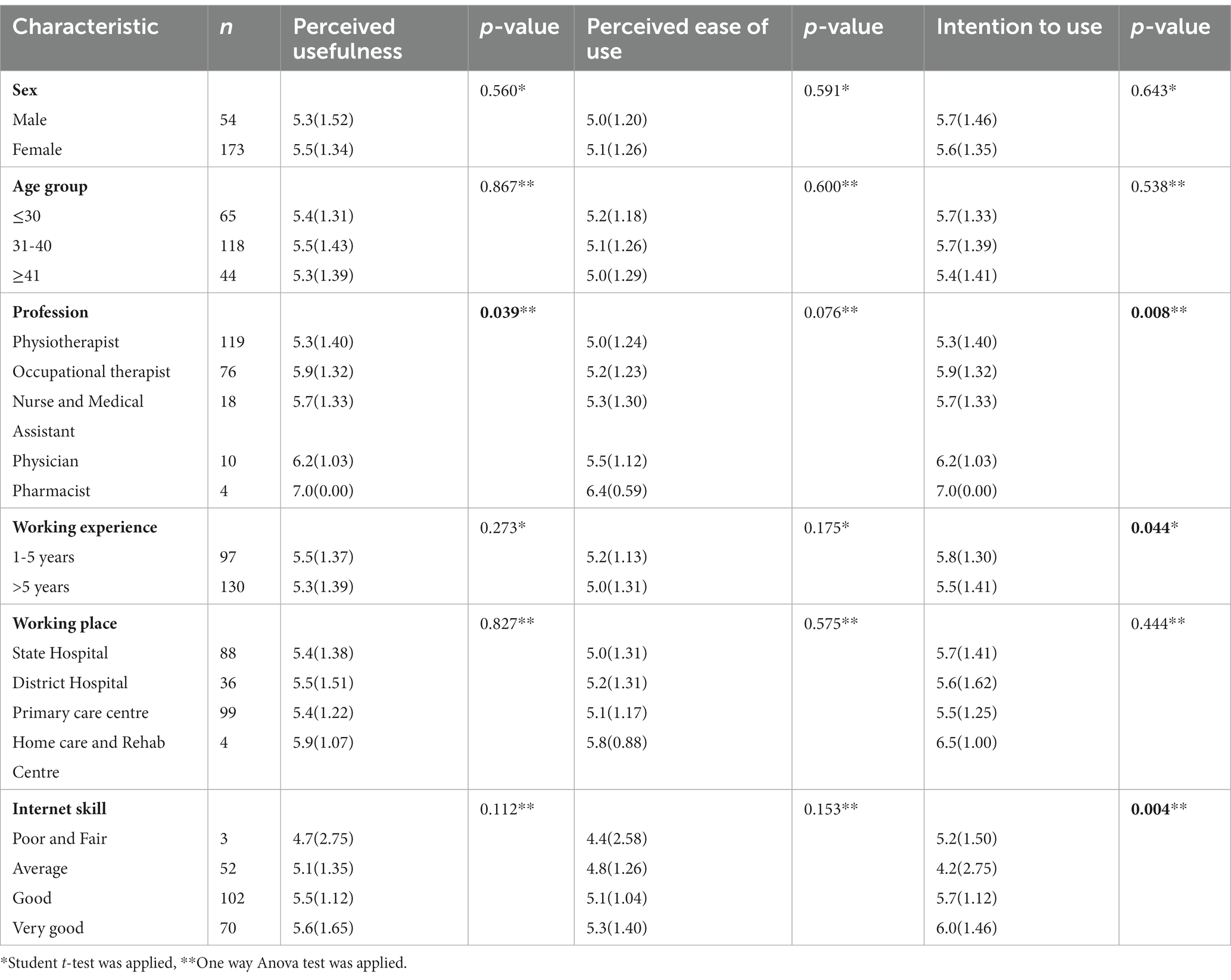
Table 3. Mean score analysis for each TAM domain by the subgroups of the study participants, based on sex, age group, profession, working experience group, working place, and internet skill (n=227).
3.2. mHealth apps acceptability and expectation
Regarding the “Stroke” mHealth app acceptability, Table 4 illustrates the joint display of both components with four key findings: (i) QUAL analysis revealed three subthemes related to the TAM model (perceived usefulness, perceived ease of use, and intention to use); (ii) three-quarters of respondents agreed that the “Stroke” mHealth app is perceived to be useful; (iii) two-quarters of respondents agreed that the “Stroke” mHealth app is perceived as easy to use and welcome using it; and (iv) more than four-fifths have the intention to use the “Stroke” mHealth app.
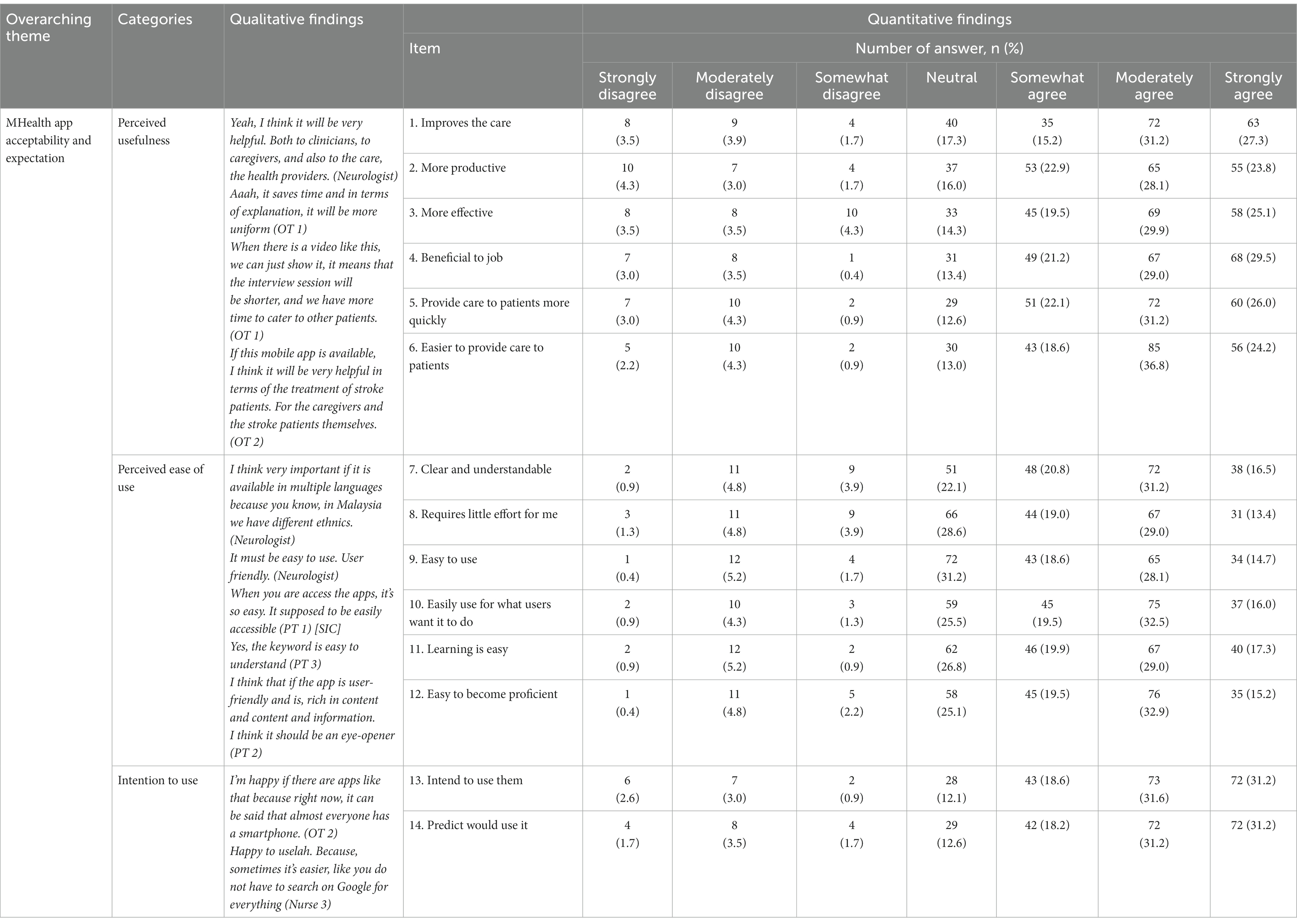
Table 4. Joint display of healthcare provider acceptability toward “Stroke” mHealth app.
3.3. Key Features of mHealth App
This section explains the expectations of healthcare providers that emerged from the qualitative component. The following three subthemes were developed: (i) availability of services for caregivers, (ii) provision of knowledge skills, and (iii) supporting caregivers in managing stroke patients. The details of the subthemes, codes, and quote examples are presented in Table 5.
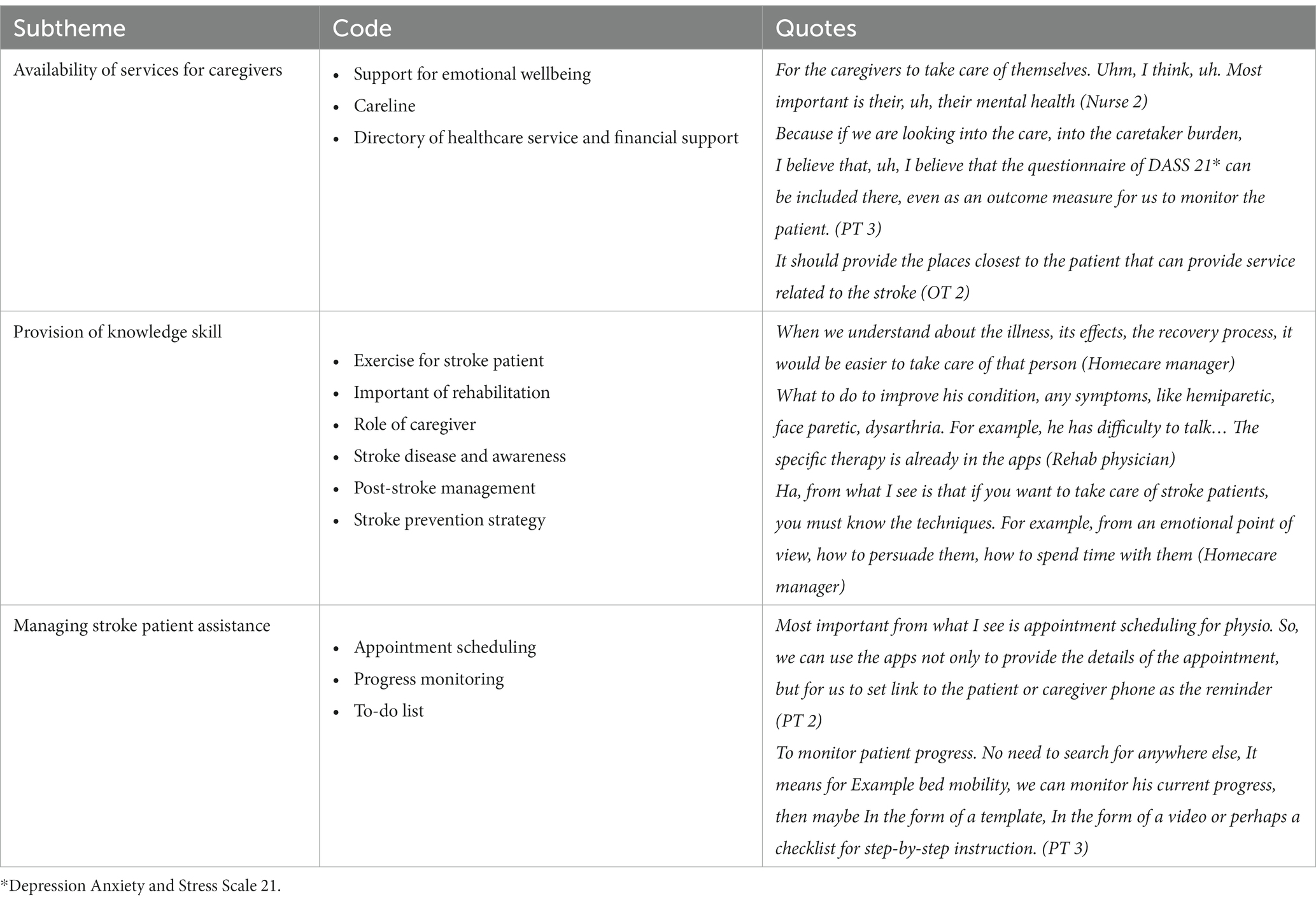
Table 5. Subtheme and codes for key features of the mHealth for caregiving theme
3.3.1. Availability of services for caregivers
The most common caregiver service addressed by participants was support for emotional wellbeing. A few methods suggested by the participants were linked to counseling therapy, peer support groups, respite care availability, and a spiritual and holistic approach.
The care line or helpdesk service was also felt to be necessary for caregivers who required urgent clarification or assistance in managing the patient. Finally, they requested the directory of healthcare-related services, such as emergency and ambulance directories, home care support, and physiotherapy services, to assist them should they require such support. To ease the burden on caregivers, a few participants believed that this app could be a decent platform for financial assistance by providing an external link to respective agencies.
3.3.2. Provision of knowledge skill
Most respondents stressed the need to provide caregivers with information from a reliable and reputable source to help them adjust to their new responsibilities. The information suggested was about exercises for stroke patients, the importance of rehabilitation, the caregiver’s role, and education regarding stroke disease and awareness. A few contributors also highlighted post-stroke management, such as stroke complications, danger signs to monitor for stroke prevention strategies, and managing patient comorbidities. In addition, some believed that the approach or strategy for comprehending the patient’s emotions and how to manage them should be included in the app.
3.3.3. Supporting caregivers in managing stroke patients
Appointment scheduling integration was one of the aspects highlighted by the participants. One participant expressed an issue that is commonly faced by caregivers, which is encountering difficulties in contacting the right department to reschedule an appointment, resulting in caregivers having to travel a long distance to schedule another appointment. Since the percentage of patients who defaulted on rehabilitation clinic follow-up was significant and there was insufficient staff to follow up with defaulters, appointment reminders were also frequently mentioned by participants.
Specifically, for the recovery process, some participants anticipated that the app would include progress monitoring. This functionality is valuable to healthcare providers for assessing and monitoring patients’ progress and is beneficial to patients with multiple caregivers. In addition, they proposed a reminder or to-do list to ensure that they do not forget the daily tasks that a stroke survivor must complete, such as rehabilitation exercises for stroke recovery.
4. Discussion
To the best of our knowledge, this is the first study to employ a mixed-methods research design to explore the acceptability and expectations of healthcare providers regarding mHealth app implementation aimed at supporting caregivers. In contrast to previous studies (21, 22, 40, 41), a comprehensive approach was adopted to establish a framework that was both generalizable and insightful (29).
Regarding individual variation in the quantitative component, in line with previous studies (25, 27), perceived usefulness, perceived ease of use, and intention to use among healthcare providers towards the mHealth app were not influenced by sex and age. However, professionals, particularly physicians and pharmacists, were more prone to use the app than their counterparts. This trend might be attributed to the increasing utilisation of mHealth apps in their daily routines (7, 25, 27). In addition, participants with more years of experience in stroke care were also shown to have greater intention towards implementing the app. With longer working experience, and being a firsthand witness, healthcare providers become more familiar with the challenges and complexities faced both by the stroke patient and their caregivers, as well as the unmet needs of caregivers over time (10, 13). These experiences can drive the intention to adopt innovative solutions like mHealth apps that have potential benefits to fill the gaps in support.
The present study revealed two important findings: (i) most healthcare providers accepted and supported the introduction of the mHealth app in assisting stroke caregivers, proven by the fact that more than 80% had the intention to use it, more than 70% perceived mHealth to be useful, and more than 60% perceived mHealth to be easy to use and (ii) the two themes derived from the qualitative method were mHealth app acceptability and expectation and the key features of mHealth for caregiving. Our findings will contribute to the existing body of knowledge on the gap between healthcare providers’ acceptability and expectations toward the implementation of mHealth apps in assisting stroke caregivers.
The high acceptability among Malaysian healthcare providers of mHealth applications in assisting stroke caregivers may stem from their potential to streamline healthcare delivery, alleviate the burden on healthcare providers, and improve public health outcomes through more direct and efficient intervention. This, in turn, can enhance the quality of care and align it with the expectations of the target community (24, 40, 45, 46). Several barriers to healthcare access during the recent COVID-19 pandemic, such as public anxiety that accessing a hospital might be unsafe, movement restrictions, and financial constraints, probably boosted healthcare providers’ acceptability of digital care interventions (13, 47). Acceptability is further reinforced by the adoption of a diverse range of digital technology and mobile health (mHealth) apps in their daily practices (25, 48). This is supported by the findings of the present study, which showed that two-thirds of the participants possessed proficient internet skills. The present study revealed that two-thirds of the participants possessed proficient internet skills, and those with better skills exhibited a significantly more intention to adopt the mHealth app.
Further exploration of the qualitative components revealed an additional theme for this study, which resolves the key features of the mHealth app for stroke caregiving. To ensure that this app is valuable and sustainable, the participants mentioned the must-have features for the app developer to incorporate: (i) availability of services for caregivers; (ii) provision of knowledge skills; and (iii) support for caregivers in managing stroke patients, which are closely related to the first theme: mHealth app acceptability and expectations.
Regarding the availability of services for caregivers, the features mentioned by the study participants were comparable to those in previously published reviews (17, 18). However, they emphasized the need for a healthcare service directory to connect caregivers with essential assistance, such as ambulance and home care services, as well as the importance of financial support due to significant expenses related to patient wellbeing, which is consistent with the findings of a local study on stroke management mobile applications for informal caregivers (49).
For the provision of knowledge skills, besides stroke recovery and exercise, participants also felt it was essential to include information on stroke awareness and the caregivers’ role. This is because the disease remains the third most prevalent cause of death and disability throughout the years, there is an increasing number of young stroke patients in Malaysia, and there is a lack of caregiver contribution recognition (1, 50–52). To support caregivers in managing stroke patients, as in previous studies, the integration of appointment scheduling, progress monitoring, and to-do lists was among the features to ensure and promote caregiver engagement (17, 18).
5. Limitations
This study has several limitations, which provide opportunities for future research. First, because the availability and accessibility of stroke-related services vary across different regions of the country, selecting healthcare providers from the northeast peninsula may restrict the generalizability of the findings to represent all healthcare providers in Malaysia. Nevertheless, the stroke clinical practice guidelines followed by healthcare providers for stroke management are standardized throughout the country; hence, findings from interviewing northeastern healthcare providers are still relevant and beneficial to targeted users.
Additionally, the present study revealed an uneven demographic distribution of healthcare providers in the northern peninsular region; the higher proportion of women shown is consistent with the gender proportion of healthcare providers in Malaysia (53). Nonetheless, given that our research is primarily aimed at evaluating the feasibility of the mHealth app, our findings remain pertinent and valid.
Finally, when using an online platform, it can be challenging to avoid sampling problems such as self-selection bias (54, 55). However, several measures were employed to ensure the validity of the interview process and to complement the qualitative findings with quantitative research to enhance the robustness of our results.
6. Future implication
This research contributes evidence to the implementation of digital healthcare transformation, aligning with the Malaysia 12th National Plan 2021–2025 (12MP), which aims toward the digitalization of healthcare (56). Over time, with the high acceptability of healthcare providers adopting the mHealth app as part of stroke management to assist stroke caregivers, it has the potential to enhance caregivers’ confidence and competence in managing stroke survivors. Ultimately, this will improve the quality of life for both stroke survivors and their caregivers. This development is a step toward transforming healthcare and making it more efficient for everyone concerned.
7. Conclusion
The findings revealed that most healthcare providers are looking forward to integrating this mHealth intervention into their patient care plans, owing to the key features identified in this study. However, to ensure the long-term sustainability of this intervention, future research should focus on determining the feasibility of integrating smartphone applications into the healthcare system after their development has been completed.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Malaysia Research Ethics Committee (MREC Ref: KKM/NIHSEC/P20-922), the Human Research Ethics Committee of USM (JEPeM: USM/JEPeM/20010031), and London School of Hygiene & Tropical Medicine (LSHTM) Research Ethics Committee (LSHTM Ethics Ref: 19079). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KM and SK supervised the project. NS, KM, SK, TT, and IP contributed to the conception and design of the study. NS, MR, KM, and KI contributed to the investigation. NS, MM, XC, and KM performed the statistical analysis. NS, KM, SK, TT, and IP conducted the thematic analysis. NS wrote the first draft of the manuscript. All authors contributed to the manuscript revision, read, and approved the submitted version.
Funding
Funding for this study was provided by the Newton-Ungku Omar Research Grant from the Ministry of Higher Education, Malaysia (203/PPSP/6780003) and the Medical Research Council, UK (MR/T018968/1). The study design, data collection and analysis, manuscript preparation, and decision to publish were carried out independently without involvement from the funding organizations.
Acknowledgments
The publication of this article was made possible thanks to the permission granted by the Director General of Health Malaysia and the funding provided by the Newton-Ungku Omar Research Grant. We also would like to acknowledge the hard work and dedication of all research team members and study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at:
References
1. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
CrossRef Full Text | Google Scholar
2. Chen, XW, Shafei, MN, Aziz, ZA, Sidek, NN, and Musa, KI. Trends in stroke outcomes at hospital discharge in first-ever stroke patients: observations from the Malaysia National Stroke Registry (2009–2017). J Neurol Sci. (2019) 401:130–5. doi: 10.1016/j.jns.2019.04.015
CrossRef Full Text | Google Scholar
3. Gbiri, CA, Olawale, OA, and Isaac, SO. Stroke management: Informal caregivers’ burdens and strians of caring for stroke survivors. Ann Phys Rehabil Med. (2015) 58:98–103. doi: 10.1016/j.rehab.2014.09.017
CrossRef Full Text | Google Scholar
4. National Research Council (US) Committee on the Role of Human Factors in Home Health Care. The Role of Human Factors in Home Health Care: Workshop Summary. Washington (DC): National Academies Press (US). COMMITTEE ON THE ROLE OF HUMAN FACTORS IN HOME HEALTH CARE. (2010). Available at:
Google Scholar
7. Labrique, A, Vasudevan, L, Mehl, G, Rosskam, E, and Hyder, AA. Digital health and health systems of the Future. (2018). Available at: www.ghspjournal.org
Google Scholar
8. Mao, Y, Lin, W, Wen, J, and Chen, G. Impact and efficacy of mobile health intervention in the management of diabetes and hypertension: a systematic review and meta-analysis. BMJ Open Diabetes Res Care. (2020) 8:e001225. doi: 10.1136/bmjdrc-2020-001225
CrossRef Full Text | Google Scholar
9. Prvu Bettger, J, Liu, C, Gandhi, DBC, Sylaja, PN, Jayaram, N, and Pandian, JD. Emerging areas of stroke rehabilitation research in low- and middle-income countries: a scoping review. Stroke. (2019) 50:3307–13. doi: 10.1161/STROKEAHA.119.023565
CrossRef Full Text | Google Scholar
10. Mohd Nordin, NA, Aziz, NAA, Abdul Aziz, AF, Ajit Singh, DK, Omar Othman, NA, Sulong, S, et al. Exploring views on long term rehabilitation for people with stroke in a developing country: findings from focus group discussions. BMC Health Serv Res. (2014) 14:118. doi: 10.1186/1472-6963-14-118
CrossRef Full Text | Google Scholar
11. Chimatiro, GL, and Rhoda, AJ. Scoping review of acute stroke care management and rehabilitation in low and middle-income countries. BMC Health Serv Res. (2019) 19:789. doi: 10.1186/s12913-019-4654-4
CrossRef Full Text | Google Scholar
12. Naqvi, IA, Montiel, TC, Bittar, Y, Hunter, N, Okpala, M, Johnson, C, et al. Internet access and usage among stroke survivors and their informal caregivers: cross-sectional study. JMIR Form Res. (2021) 5. doi: 10.2196/25123
CrossRef Full Text | Google Scholar
13. Sidek, NN, Kamalakannan, S, Tengku Ismail, TA, Musa, KI, Ibrahim, KA, Abdul Aziz, Z, et al. Experiences and needs of the caregivers of stroke survivors in Malaysia—a phenomenological exploration. Front Neurol. (2022) 13:996620. doi: 10.3389/fneur.2022.996620
CrossRef Full Text | Google Scholar
14. Panzeri, A, Ferrario, SR, and Vidotto, G. Interventions for psychological health of stroke caregivers: a systematic review. Front. Psychol. (2019) 10:2045. doi: 10.3389/fpsyg.2019.02045
CrossRef Full Text | Google Scholar
15. Sala-González, M, Pérez-Jover, V, Guilabert, M, and Mira, JJ. Mobile apps for helping informal caregivers: a systematic review. Int J Environ Res Public Health. (2021) 18:1–17. doi: 10.3390/ijerph18041702
CrossRef Full Text | Google Scholar
16. Lobo, EH, Abdelrazek, M, Kensing, F, Rasmussen, LJ, Livingston, PM, Grundy, J, et al. Technology-based support for stroke caregiving: a rapid review of evidence. J Nurs Manag. (2021) 30:3700–13. doi: 10.1111/jonm.13439
CrossRef Full Text | Google Scholar
17. Firmawati, E, Setyopanoto, I, and Pangastuti, HS. Mobile health application to support family caregivers in recurrent stroke prevention: scoping review. Open Access Macedonian J Med Sci. (2022) 9:142–51. doi: 10.3889/oamjms.2022.7859
CrossRef Full Text | Google Scholar
18. Lobo, EH, Frølich, A, Kensing, F, Rasmussen, LJ, Livingston, PM, Grundy, J, et al. mHealth applications to support caregiver needs and engagement during stroke recovery: a content review. Res Nurs Health. (2021) 44:213–25. doi: 10.1002/nur.22096
CrossRef Full Text | Google Scholar
20. Sureshkumar, K, Murthy, G, Natarajan, S, Naveen, C, Goenka, S, and Kuper, H. Evaluation of the feasibility and acceptability of the ‘Care for Stroke’ intervention in India, a smartphone-enabled, carer-supported, educational intervention for management of disability following stroke. BMJ Open. (2016) 6:e009243. doi: 10.1136/bmjopen-2015-009243
CrossRef Full Text | Google Scholar
21. Alexandre, B, Reynaud, E, Osiurak, F, and Navarro, J. Acceptance and acceptability criteria: a literature review. Cogn Technol Work. (2018) 20:165–77. doi: 10.1007/s10111-018-0459-1
CrossRef Full Text | Google Scholar
22. Nadal, C, Sas, C, and Doherty, G. Technology acceptance in mobile health: Scoping review of definitions, models, and measurement. J Med Internet Res. (2020) 22:e17256. doi: 10.2196/17256
CrossRef Full Text | Google Scholar
23. Leigh, S, and Ashall-Payne, L. The role of health-care providers in mHealth adoption. Lancet Digit Health. (2019) 1:e58–9. doi: 10.1016/S2589-7500(19)30025-1
CrossRef Full Text | Google Scholar
24. Bally, ELS, and Cesuroglu, T. Toward Integration of mHealth in primary care in the Netherlands: a qualitative analysis of stakeholder perspectives. Front Public Health. (2020):407:7. doi: 10.3389/fpubh.2019.00407
CrossRef Full Text | Google Scholar
25. Lim, HM, Dunn, AG, Muhammad Firdaus Ooi, S, Teo, CH, Abdullah, A, Woo, WJ, et al. mHealth adoption among primary care physicians in Malaysia and its associated factors: a cross-sectional study. Fam Pract. (2021) 38:210–7. doi: 10.1093/fampra/cmaa103
CrossRef Full Text | Google Scholar
26. Wu, P, Zhang, R, Luan, J, and Zhu, M. Factors affecting physicians using mobile health applications: an empirical study. BMC Health Serv Res. (2022) 22:24. doi: 10.1186/s12913-021-07339-7
CrossRef Full Text | Google Scholar
27. Wasti, SP, Simkhada, P, van Teijlingen, E, Sathian, B, and Banerjee, I. The growing importance of mixed-methods research in health. Nepal J Epidemiol. (2022) 12:1175–8. doi: 10.3126/nje.v12i1.43633
CrossRef Full Text | Google Scholar
28. Kaushik, V, and Walsh, CA. Pragmatism as a research paradigm and its implications for social work research. Soc Sci. (2019) 8:1–17. doi: 10.3390/socsci8090255
CrossRef Full Text | Google Scholar
29. Creswell, JW, and Plano Clark, VL. Designing and conducting mixed methods research. 3rd ed. Thousand Oaks, CA: SAGE Publications, Inc. (2018).
Google Scholar
30. Saunders, B, Sim, J, Kingstone, T, Baker, S, Waterfield, J, Bartlam, B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. (2018) 52:1893–907. doi: 10.1007/s11135-017-0574-8
CrossRef Full Text | Google Scholar
31. Williams, V, Price, J, Hardinge, M, Tarassenko, L, and Farmer, A. Using a mobile health application to support self-management in COPD: A qualitative study. Br J Gen Pract. (2014) 64. doi: 10.3399/bjgp14X680473
CrossRef Full Text | Google Scholar
32. Smirnova, E, Eriksson, N, and Fagerstrøm, A. Adoption and use of health-related mobile applications: a qualitative study with experienced users. In: HEALTHINF 2021 – 14th International Conference on Health Informatics; Part of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies, BIOSTEC, 2021. SciTePress (2021), 288–295.
Google Scholar
33. Torbjørnsen, A, Ribu, L, Rønnevig, M, Grøttland, A, and Helseth, S. Users’ acceptability of a mobile application for persons with type 2 diabetes: a qualitative study. BMC Health Serv Res. (2019) 19:641. doi: 10.1186/s12913-019-4486-2
CrossRef Full Text | Google Scholar
34. Creswell, JW, and Creswell, JD. Research design: qualitative, quantitative and mixed methods approaches. Sage Publications, Inc. (2018).
Google Scholar
35. Krejcie, RV, and Morgan, DW. Determining sample size for research activities. Educ Psychol Meas. (1970) 30:607–10. doi: 10.1177/001316447003000308
CrossRef Full Text | Google Scholar
37. Mack, N, Woodsong, C, Macqueen, KM, and Greg Guest, EN. Qualitative research methods: a data collector’s field guide. Anti Corrosion Methods Mater. (1989) 36:24–31. doi: 10.1108/eb020803
CrossRef Full Text | Google Scholar
38. Johnson, TP. Snowball sampling: introduction In: N Balakrishnan, T Colton, B Everitt, W Piegorsch, F Ruggeri, and JL Teugels, editors. Wiley StatsRef: statistics reference online (2014). doi: 10.1002/9781118445112.stat05720
CrossRef Full Text | Google Scholar
39. Lincoln, Y, Lincoln, YS, and Guba, EG. Naturalistic inquiry. Newbury Park, CA: Sage (1985).
Google Scholar
40. van der Ham, IJM, van der Vaart, R, Miedema, A, Visser-Meily, JMA, and van der Kuil, MNA. Healthcare professionals’ acceptance of digital cognitive rehabilitation. Front Psychol. (2020) 11:617886. doi: 10.3389/fpsyg.2020.617886
CrossRef Full Text | Google Scholar
41. Nunes, A, Limpo, T, and Castro, SL. Acceptance of mobile health applications: examining key determinants and moderators. Front Psychol. (2019) 10:2791. doi: 10.3389/fpsyg.2019.02791
CrossRef Full Text | Google Scholar
42. Fred, DD. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quart. (1989) 13:319–40. doi: 10.5962/bhl.title.33621
CrossRef Full Text | Google Scholar
43. Braun, V, and Clarke, V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
CrossRef Full Text | Google Scholar
44. Fetters, MD, Curry, LA, and Creswell, JW. Achieving integration in mixed methods designs – principles and practices. Health Serv Res. (2013) 48:2134–56. doi: 10.1111/1475-6773.12117
PubMed Abstract | CrossRef Full Text | Google Scholar
45. Meyer, AJ, Armstrong-Hough, M, Babirye, D, Mark, D, Turimumahoro, P, Ayakaka, I, et al. Implementing mhealth interventions in a resource-constrained setting: case study from Uganda. JMIR Mhealth Uhealth. (2020) 8:e19552. doi: 10.2196/19552
CrossRef Full Text | Google Scholar
46. Lingg, M, and Lütschg, V. Health system stakeholders’ perspective on the role of mobile health and its adoption in the swiss health system: qualitative study. JMIR Mhealth Uhealth. (2020) 8:e17315. doi: 10.2196/17315
CrossRef Full Text | Google Scholar
47. Haji Mukhti, MI, Ibrahim, MI, Tengku Ismail, TA, Nadal, IP, Kamalakannan, S, Kinra, S, et al. Family caregivers’ experiences and coping strategies in managing stroke patients during the COVID-19 pandemic: a qualitative exploration study. Int J Environ Res Public Health. (2022) 19:942. doi: 10.3390/ijerph19020942
CrossRef Full Text | Google Scholar
48. Malaysian Communications and Multimedia Commission. Communications and multimedia: pocket book of statistics, a half yearly statistical bulletin of the communications and multimedia industry. (2021). Available at:
Google Scholar
49. Haji Mukhti, MI, Ibrahim, MI, Tengku Ismail, TA, Nadal, IP, Kamalakannan, S, Kinra, S, et al. Exploring the need for mobile application in stroke management by informal caregivers: a qualitative study. Int J Environ Res Public Health. (2022) 19:12959. doi: 10.3390/ijerph191912959
CrossRef Full Text | Google Scholar
50. Ahmad Zubaidi, ZS, Ariffin, F, Oun, CTC, and Katiman, D. Caregiver burden among informal caregivers in the largest specialized palliative care unit in Malaysia: a cross sectional study. BMC Palliat Care. (2020) 19. doi: 10.1186/s12904-020-00691-1
CrossRef Full Text | Google Scholar
51. Jawahir, S, Tan, EH, Tan, YR, Mohd Noh, SN, and Ab, RI. The impacts of caregiving intensity on informal caregivers in Malaysia: findings from a national survey. BMC Health Serv Res. (2021) 21:391. doi: 10.1186/s12913-021-06412-5
CrossRef Full Text | Google Scholar
52. Tan, KS, and Venketasubramanian, N. Stroke burden in Malaysia. Cerebrovasc Dis Extra. (2022) 12:58–62. doi: 10.1159/000524271
CrossRef Full Text | Google Scholar
54. Nayak, MSDP, and Narayan, KA. Strengths and weaknesses of online surveys. IOSR J Hum Soc Sci.. (2019) 24:31–38. doi: 10.9790/0837-2405053138
CrossRef Full Text | Google Scholar
link







