Innovative mobile app solution for facial nerve rehabilitation: a usability analysis

Introduction
Facial palsy (FP), irrespective of its idiopathic, infectious, traumatic or iatrogenic etiology, can be an incisive life event for patients resulting in a reduced physical and mental quality of life (QoL) (1–4). Besides cause-related treatments (e.g., antiinfective therapy for bacterial or viral causes, corticosteroids), a regular training of the facial muscles is usually conducted by the patients themselves, in order to reduce the described limitations in QoL and to achieve fast facial nerve regeneration (5–7). However, missing or significantly reduced movements of the paretic side can lead to a decrease in the patient’s motivation for daily, home-based training. In addition, insufficient or inadequate instructions can lead to the development of incorrect movement patterns, which might trigger an impaired healing resulting in so-called synkinesia (8).
The broad availability of smartphones and therefore also the use of medical application software (apps) enables its implementation in the field of rehabilitation and to supplement traditional treatment and training methods (9–11). Exercises can be instructed, a personalized therapy plan can be created and, most importantly training can be reminded. In addition, good accessibility of apps can help to overcome the potential shortage of physical and logopedic therapy in facial palsy caused by long distances and an inadequate number of therapists (12). Nevertheless, the training progress can be monitored by the therapists at regular intervals in addition to the use of an app.
While there are a couple of apps for grading facial palsy (13, 14), so far there are only few apps aiming to train facial function in case of a palsy, some of which offer limited options. Extensive distribution and proof of an advantage over previous therapies are completely lacking. For this reason, a specific app (FACEsemper) for training of facial palsy was developed as the fundament for this study. The aim of the present study is to evaluate the usability of the FACEsemper app before it might be used in larger patient groups. Potential malfunctions or opportunities for improvement are to be detected and the app adapted accordingly.
Methods
Study cohort
In total, 10 healthy subjects, 9 FP patients, and 8 physicians of the disciplines neurology, neurosurgery and plastic-reconstructive surgery gave their written informed consent and completed the study. The participating patients were recruited at the Department of Neurosurgery and Neurotechnology at the University Hospital of Tuebingen. Inclusion criterion for the patient group was the presence of a peripheral facial palsy following a tumor resection in the cerebellopontine angle (CPA). A further criterion for participation among all groups was possession of an Android smartphone, as the primary app development was performed in the Android operating system, and a transfer to the iOS operating system was planned only after usability testing and the determination of necessary changes. Exclusion criteria included treatment with Botulinum toxin in the last 6 months, facial piercings/implants and the inability to operate a smartphone independently. In addition to patients with facial palsy, healthy subjects and physicians were included in order to identify interface issues or user experience barriers that are not specific to the patient’s medical condition (e.g., confusing navigation, unclear instructions) as well as to ensure that the app aligns with medical standards and therapeutic goals. For this purpose, only physicians who have regular contact with FP patients were included. The study was carried out in accordance with the recommendations of the ethics committee of the Eberhard Karls University Tuebingen (732/2021BO1) and conducted in accordance with the declaration of Helsinki.
Software development and app functions
The FACEsemper app was designed by a software developer in close collaboration with a team of neurosurgeons from the University Hospital of Tuebingen who are familiar with postoperative facial palsies following tumor resection of the CPA. The app is built using Flutter, an open-source framework developed by Google (Google Inc., Mountain View, California, USA) (15). The programming language used within the flutter ecosystem is called Dart. One of the main advantages of using a framework like flutter is that it can be used to build multi-platform applications. That means, the majority of the codebase has to be written only once but can be deployed on different platforms like iOS or Android. However, for low-level or platform-specific functionality, native code is still required to interact with the respective interfaces. Additionally, we integrated several external libraries to provide essential functionalities such as sending notifications, playing a video, or opening a file dialog to export the training results. A full list of dependencies, including version information and license details, is available within the app.
FACEsemper offers three training programs including daily training, programs for specific regions, and individual training sessions (Figure 1). When setting up the “daily training” program, the therapist and patient can determine the intensity of the training of each part of the face (i.e., forehead, eye, mouth) and whether additional synkinesia training should be performed. Based on the selected settings, various exercises for the face are randomly compiled by the app (e.g., strong eye closure, horizontal facial stretching). In the category of “specific training”, individual facial areas can be selected and the app creates a complete training program for the selected region. In addition, the user can choose individual exercises by using the “individual training” function (Figure 1).
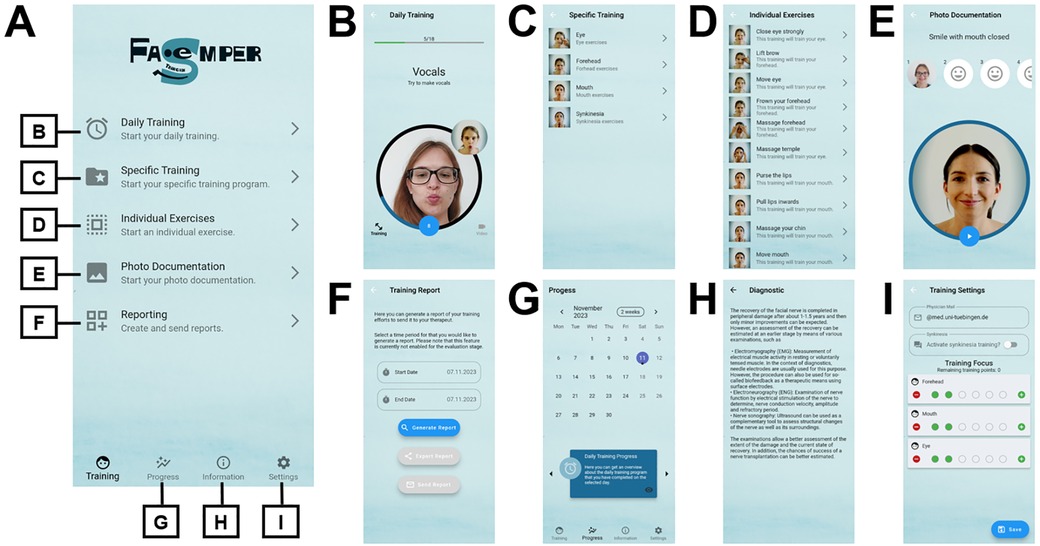
Figure 1. Structure of the FACEsemper app. (A) After initial setup, a welcome page is shown to the user. The app functionalities presented in B-I can be opened via specific buttons. (B) demonstrates one exercise of the daily training. In the large circle, the user’s face is captured and displayed via the camera. Furthermore, video instructions for the exercise are displayed in the small circle. (C,D) show the specific and individual exercises. (E) Photo documentation is provided in a standardized form of 6 facial expressions. (F) Training reports can be sent for improved patient-therapist communication. (G) A calendrical summary showing the exercise units and photo documentation gives the user an overview of their training status. (H) demonstrates one of the information sides and (I) shows the functions of the training settings.
Additional functionalities include a reminder function for the daily training, photo documentation, a calendrical overview of the training progress, the generation of a training report for a therapist and an information page where users can gain further knowledge about facial palsies approved by a medical doctor (e.g., causes or diagnostic methods). The visualization of the training progress includes both the frequency of the exercises performed and the photo documentation. Within the training report, the user can independently select which training sessions and photo documentation are sent to the therapist. Automated data transmission was not implemented to ensure patients’ privacy rights.
Usability evaluation
In order to provide reliable evaluation, FACEsemper was tested by the participants over a period of 2 weeks. They were given the following tasks: (1) setting up the app with configuring the language and the reminder; (2) adjusting the training settings by determining the parts of the face to be trained and activating/deactivating synkinesia training; (3) performing the daily facial training for 2 weeks; (4) completing a photo documentation after each training week; (5) checking the training progress in the calendar; (6) creating and sending a training report after each training week; (7) reading the information material.
After testing and performing the aforementioned tasks, the participants completed several questionnaires to assess the usability of the FACEsemper app: mHealth App Usability Questionnaire for standalone apps (MAUQ); System Usability Scale (SUS); Visual Aesthetics of Apps Inventory (VisAAI); FACEsemper-specific evaluation questionnaire. In addition, training reports sent by the participants, were analyzed to determine how often the app was used and whether the photo documentation was completed.
The MAUQ for standalone apps is used to evaluate app functions regarding medical benefits and ease of use. It consists of a total of 18 questions, which can be assigned to the categories ease of use (5 items), interface and satisfaction (7 items) and usefulness (6 items). Each item can be rated from 1 (strongly disagree) to 7 (strongly agree). A mean value is calculated from all items together for the assessment (16). For this study we used the “MAUQ for Healthcare Providers” in the group of physicians and the “MAUQ for Patients” in the groups of patients and healthy subjects.
The SUS consists of 10 items and evaluates app-usability particularly in terms of ease-of-use and efficiency. The items are rated on a 5-point Likert scale from 0 (disagree) to 4 (agree). After converging the values, summing the individual items and multiplying by 2.5, the absolute SUS score can be assigned to a value of 0–100. A higher value indicates a better rating, with a value of ∼68–80 corresponding to a good rating and >80 to an excellent rating (17).
The VisAWI evaluates the aesthetics of websites with the categories simplicity (5 items), diversity (5 items), colorfulness (4 items) and craftsmanship (4 items). Each of the 18 items is rated by the user on a Likert scale from 1 (strongly disagree) to 7 (strongly agree). After re-encoding negatively polarized items, the individual scale values are added to form the scale mean of each category and then the sum is divided by the number of items in the category. The overall mean value of the VisAWI is obtained by summing all subscale values and then dividing by 4 (18). For aesthetic evaluation of the FACEsemper app we used an adjusted version of the VisAWI (VisAAI) by replacing “website” with “app” in the questionnaire.
The FACEsemper-specific questionnaire assessed the following categories of the app separately: attitudes (4 items), training (4 items for healthy subjects and patients, 5 items for physicians), calendar (3 items), photo documentation (3 items), information (2 items for healthy subjects and patients, 3 items for physicians), training report (2 items), workflow (3 items). These items could be rated by the user from 1 (strongly disagree) to 7 (strongly agree). Finally, subjects were able to give an overall assessment of the app in the categories of content, user-friendliness, aesthetics and overall impression with values from 1 (very satisfactory) to 5 (unsatisfactory) (Table 1, FACEsemper specific questionnaire total value) and provide open feedback.
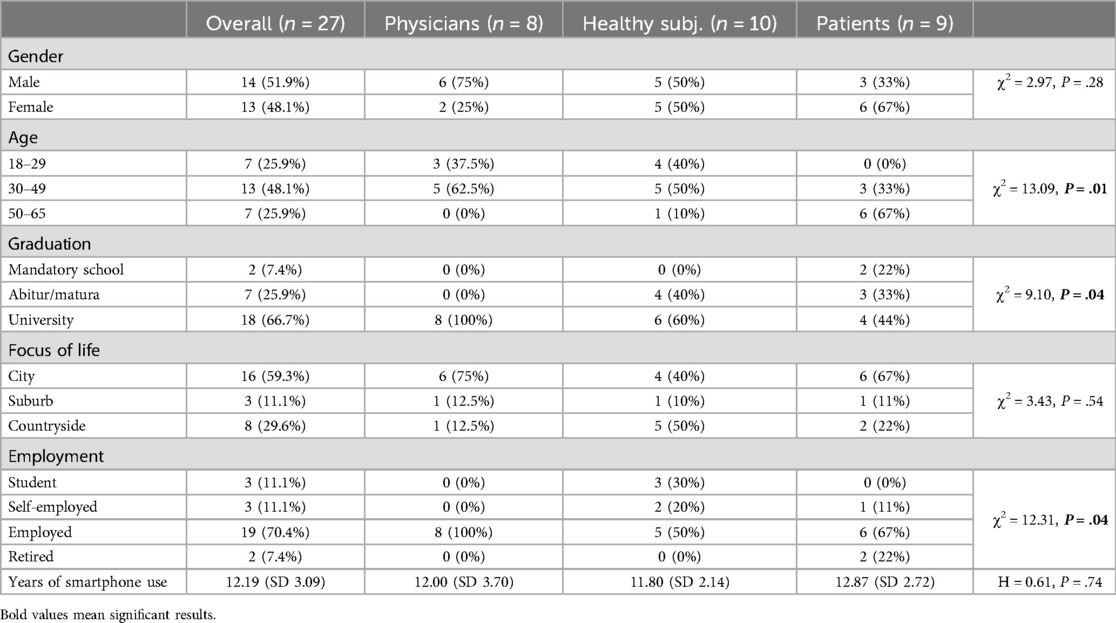
Table 1. Participant characteristics.
Statistics
To acquire data for statistical analysis, and to create info graphics SPSS (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp.) was used. An a priori case number calculation has been performed. To analyze nominally-scaled data we used the Chi-squared test and analyzed non-nominally distributed data employing the Kruskal-Wallis test. The data are shown as mean values (SD). P-values <0.05 were considered significant (confidence interval 95%). Demographic data were collected solely for descriptive statistics because of the inclusion criteria for physicians, which resulted in selection bias.
Results
Participant characteristics
A total of 27 subjects (i.e., 8 physicians, 9 patients with facial palsy and 10 healthy subjects) prospectively evaluated the usability of the FACEsemper app for the entire two weeks and therefore completed the study. 48.1% of participants (13/27) were female and 48.1% were between 30 and 49 years of age (13/27). Results demonstrated differences between the groups in terms of age, education level and employment status. There were no differences in age and primary residency. Moreover, participants in all groups reported using a smartphone for more than 10 years (Table 1). 40.7% of participants (11/27) have previously used a fitness app.
Training
A total of 290 (SD 163) exercises were performed by each participant. Patients performed significantly more exercises (mean 459, SD 210) than physicians (mean 221, SD 54) and healthy subjects (mean 213, SD 40, H = 8.11, P = .02). During the test period, 2.2 (SD 1.8) training reports were created and 2.0 (SD 0.7) photo documentations were performed by each individual. No difference in the number of reports (H = 2.63, P = .27) or photo documentations (H = 1.17, P = .56) was found between the groups.
Usability of the FACEsemper app
All participants completed the evaluation via three validated questionnaires and an app-specific questionnaire. The mean scores of the whole cohort and its subgroups are listed in Table 2. SUS scores were highest in patients and lowest in physicians. However, this difference was not statistically significant. For the VisAAI, scores between the four categories varied only slightly and showed the highest values for craftmanship (mean 6.3, SD 0.6) and lowest values for diversity (mean 5.3, SD 1.1) with no statistically significant difference between the groups of participants. Overall, the app was evaluated with good or excellent scores by all three groups (Figure 2).
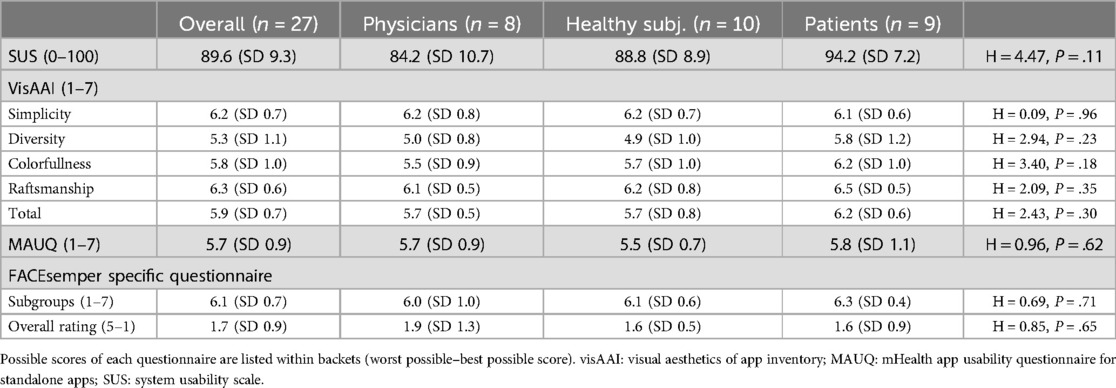
Table 2. Usability ratings of participants.
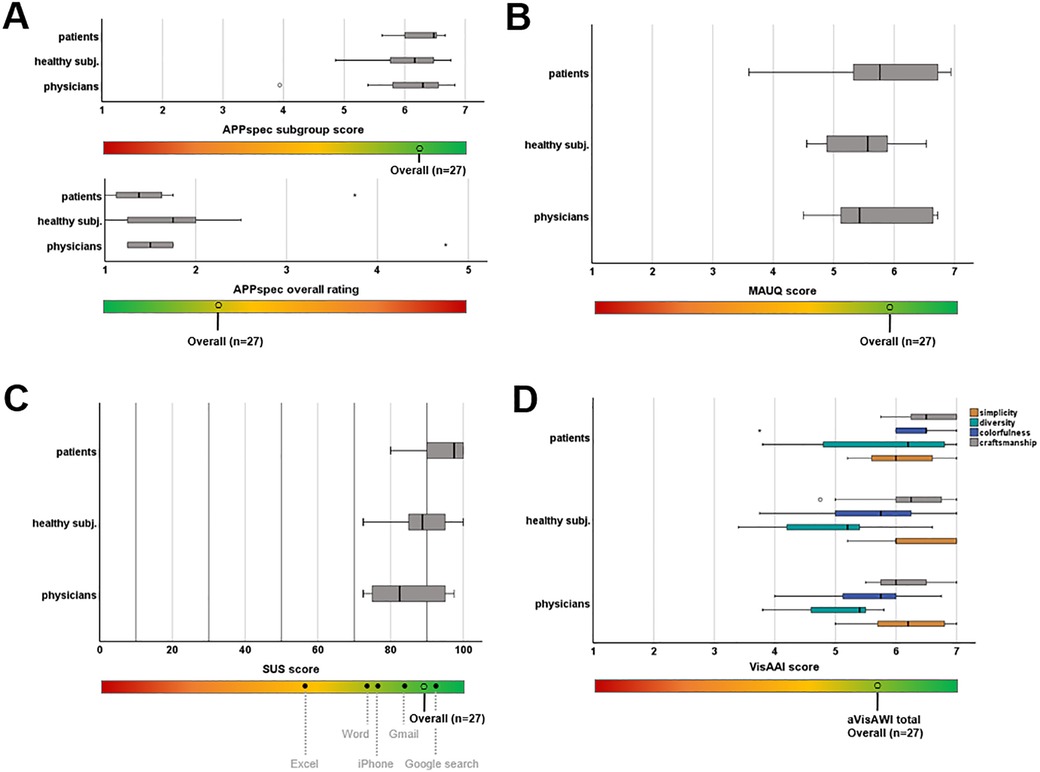
Figure 2. Usability evaluation by different rating scales. (A) FACEsemper specific questionnaire; (B) mHealth app Usability Questionnaire for standalone apps (MAUQ); (C) System Usability Scale (SUS) values are compared with SUS values of everyday products published by Kortum et al. (19); (D) Visual Aesthetics of Apps Inventory (VisAAI).
Participants’ suggestions for improvement
In total, 15/27 subjects used the opportunity to provide qualitative feedback. The analysis of the this data revealed that in particular the reminder function did not work properly. One user recommended the implementation of a reminder several times a day. Apart from a training reminder, a voluntary reminder function for creating photo documentation and the training report were suggested by several users. In addition to a visual signal, the participants also requested an acoustic signal at the end of a task so that they could receive feedback about the end of the task during exercises that involved closing their eyes. One subject asked to customize the navigation in the progress area as he did not find it intuitive. However, no specific adaptation recommendations were provided. However, the overall conclusion of the patients was positive, and it was repeatedly expressed that they would be happy to continue using the app after the end of the study. One patient wrote in this context: “By the way, I will continue to use the app. […] Overall, it helps me to practice more regularly, and the random selection of exercises is good, so there are always new stimuli”.
Discussion
Statistical calculations suggest that 6.9 billion smartphones are in use worldwide in 2024. In Germany even 88.1% of all households are equipped with a smartphone according to the Federal Statistical Office (20). This also raises the possibility of supplementing traditional treatment methods in the medical field with the use of apps, e.g., in the rehabilitation of neurological function. Apps can provide support in different aspects: information, health habits, assessment, treatment, and specific uses (21). Previous studies in various diseases have demonstrated that the use of medical mobile applications can increase the self-efficacy of patients and at the same time, improved self-efficacy leads to an improved overall condition and physical function in patients with paresis after stroke (22–25). An improvement of rehabilitation through mobile applications is therefore also plausible for patients with FP.
In this context, the presented usability study of the FACEsemper app for training in patients with FP showed positive feedback with very good usability ratings. SUS is the most commonly used usability score to rate eHealth applications (17). Applications are considered acceptable in case of SUS scores >70 and as excellent if higher than 85 respectively (26). FACEsemper was overall rated excellent according to this scoring system. This becomes particularly obvious when comparing the SUS rating of FACEsemper in relation to everyday products such as Excel (mean SUS score 56.5, SD 18.6), Word (mean SUS score 76.2, SD 15.0) or Amazon (mean SUS score 81.8, SD 14.8) (19). Furthermore, a cut point analysis of the VisAWI showed that a score of 4.5 or higher should be aimed for new designs (27). VisAAI scores in the presented study exceeded this cut point in all subcategories and groups of participants reflecting a pleasant aesthetic design of the app. The overall rating score was 1.7, which shows a result between very satisfactory (=1) and rather satisfactory (=2).
The MAUQ questionnaire was utilized in both its patient and healthcare professional versions. The scores among patient groups and healthy individuals who completed the patient version, as well as the physicians who filled out the health professional version, were comparable. Furthermore, the physicians did not provide any suggestions for modifications or additional functions related to the app’s medical content. Consequently, we conclude that these professionals, who regularly treat patients with facial palsy, offer a positive validation of the app. Moreover, the qualitative evaluation of patient feedback and the significantly more frequent use of the app by patients compared to the other two study groups suggests a genuine need for targeted features in facial rehabilitation. This higher usage could be due to patients experiencing greater benefit due to their immediate rehabilitation needs. While the study did not explicitly examine the specific motivations for higher app use by patients, it is likely that their immediate therapeutic needs led to greater engagement. Previous studies have shown in this context that there is a lack of therapeutic care for FP patients by means of specialized therapy (e.g., physiotherapy) and that 10% of patients need to travel up to more than >115 miles (=185 km) just to receive specific therapy (12, 28).
There are already other apps that have been developed for the purpose of facial training (e.g., “face2face- facial exercises”, “Face it!” and “FaceRehab”). A special feature of the face2face app is its use of an augmented reality mask during facial exercises, allowing patients to avoid constantly viewing their paretic face. This can have the advantage of maintaining motivation for practicing. On the other hand, it can also be annoying for the patient not to receive realistic feedback. The FaceRehab app, available for purchase and primarily designed for patients with Bell’s palsy, offers very similar functions to the app presented (e.g., progress tracking, reminders, training plan) (29). One difference to the presented app that should be emphasized is that it contains an analysis function that determines certain viewpoints for assessing asymmetry. While this feature can provide a more objective evaluation of the rehabilitation process, it also carries the risk of patients becoming overly focused on their perceived deficits. This preoccupation can lead to demotivation, especially if they do not see immediate changes over several days or weeks. Therefore, it might be beneficial for therapists to conduct this type of analysis at designated intervals rather than having patients do it themselves. Furthermore, a) some of these apps are no longer available via the App or Play store and b) we are not aware of any studies on usability investigation or testing of an advantage compared to a therapy without the app support. Only one study by Taeger et al. (14) describes the process of developing an app, which describes similar functions/possibilities within the app, but is also not available to the public at the moment (30).
FACEsemper already includes multiple features, such as an individualized daily therapy plan, monitoring of rehabilitation progress and information about the disease (30–34). Data security and privacy aspects have also been taken into account during development, as this is an important factor in any medical care app (35, 36). Our usability evaluation demonstrated that the reminder function implemented so far is desired by patients but is still unreliable. We decided to not update the app during the study to avoid changes that could have an impact on other parts and thus potentially hinder comparison of the test results. We will resolve the issue in the next version by debugging the root cause. As recommended by the patients, we will integrate reminder functions for the photo documentation and training report as well as an acoustic signal at the end of a task so that patients could receive feedback about the end of the task. Further ideas and plans in future versions are a) to include communication with the therapist via a video consultation (in addition to the exclusive communication via the training reports), b) incorporate self-rating tools to capture the self-perceived impairment caused by facial palsy, as well as c) gamification elements (e.g., virtual coins and gadgets). Finally, the possibility of voluntary networking of FP patients will be evaluated.
Limitations
The study’s overall validity is limited by the small sample size of 27 participants, including only 9 patients with facial palsy. This may restrict the generalizability of our findings, especially as the heterogeneity of patients with facial palsy (e.g., reason and extent of facial palsy, patient’s age, gender and ethnicity) was not considered in this way. A larger sample size would enhance statistical power and enable more robust analyses, which is crucial for assessing the treatment effects of the app in the future. This would help identify meaningful differences in recovery rates and improve the study’s external validity. To achieve a sufficiently diverse patient population, a multi-center study involving various specialties—such as neurosurgery, neurology, ENT, and plastic surgery—would be a beneficial approach. However, previous usability studies already showed reliable results with 8–10 subjects in the assessment of the SUS questionnaire and in usability studies in general (37, 38). Furthermore, the consistent ratings in all groups indicate a usable result of the present study.
A further limitation is the fact that the data collected does not provide any information about the therapeutic benefits of the app for facial rehabilitation or the long-term usability. This is due to the test duration of two weeks, which allows evaluating the usability with regard to the described aspects such as simplicity or craftmanship as well as the basic functions of the app (e.g., photo documentation and report), but not with regard to the therapeutic effect. Future studies should extend the follow-up duration and also include a control group receiving standard physical therapy without the app to better evaluate the app’s effectiveness in promoting long-term recovery and user engagement. These studies should also include objective measurement techniques to measure the facial palsy and its recovery (e.g., Sunnybrook scale or eFACE scale) (39–41).
Conclusion
This study shows that the developed prototype of the FACEsemper app meets the requirements of a mobile application regarding usability, visual aesthetics and patient feedback was excellent. One aim of this study was to identify possible malfunctioning and detect additional necessary features which will be implemented in future FACEsemper versions. As a next step, app based facial training in addition to common therapy will be validated in a prospective randomized controlled clinical trial on patients with facial palsy of various causes. The planned follow-up study will focus on the duration until rehabilitation of the FP, the degree of rehabilitation achieved, and adherence to training over a twelve-month period. This will be compared between patients using an app-based training program combined with standard training and those using standard training alone.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Eberhard Karls University Tuebingen (732/2021BO1). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KM: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft. ML: Methodology, Software, Validation, Writing – original draft, Writing – review & editing. CR: Validation, Writing – review & editing. GN: Validation, Writing – review & editing. MT: Validation, Writing – review & editing. HH: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CPA, cerebellopontine angle; FP, facial palsy; MAUQ, mHealth app usability questionnaire for standalone apps; QoL, quality of life; SUS, system usability scale; VisAAI, visual aesthetics of apps inventory (adjusted version of the VisAWI); VisAWI, visual aesthetics of websites inventory.
References
1. Cross T, Sheard CE, Garrud P, Nikolopoulos TP, O’Donoghue GM, Sheard C E, et al. Impact of facial paralysis on patients with acoustic neuroma. Laryngoscope. (2000) 110(9):1539–42. doi: 10.1097/00005537-200009000-00024
PubMed Abstract | Crossref Full Text | Google Scholar
2. Verhoeff R, Bruins TE, Ingels KJAO, Werker PMN, van Veen MM. A cross-sectional analysis of facial palsy-related quality of life in 125 patients: comparing linear, quadratic and cubic regression analyses. Clin Otolaryngol. (2022) 47(4):541–5. doi: 10.1111/coa.13934
PubMed Abstract | Crossref Full Text | Google Scholar
3. Machetanz K, Lee L, Wang SS, Tatagiba M, Naros G. Trading mental and physical health in vestibular schwannoma treatment decision. Front Oncol. (2023) 13:1152833. doi: 10.3389/fonc.2023.1152833
PubMed Abstract | Crossref Full Text | Google Scholar
4. Nellis JC, Ishii M, Byrne PJ, Boahene KDO, Dey JK, Ishii LE, et al. Association among facial paralysis, depression, and quality of life in facial plastic surgery patients. JAMA Facial Plast Surg. (2017) 19(3):190–6. doi: 10.1001/jamafacial.2016.1462
PubMed Abstract | Crossref Full Text | Google Scholar
5. Pereira LM, Obara K, Dias JM, Menacho MO, Lavado EL, Cardoso JR. Facial exercise therapy for facial palsy: systematic review and meta-analysis. Clin Rehabil. (2011) 25:649–58. doi: 10.1177/0269215510395634
PubMed Abstract | Crossref Full Text | Google Scholar
6. Cardoso JR, Teixeira EC, Moreira MD, Fávero FM, Fontes SV, Bulle De Oliveira AS. Effects of exercises on bell’s palsy: Systematic review of randomized controlled trials. Otol Neurotol. (2008) 29:557–60. doi: 10.1097/MAO.0b013e31816c7bf1
PubMed Abstract | Crossref Full Text | Google Scholar
7. Van Landingham SW, Diels J, Lucarelli MJ. Physical therapy for facial nerve palsy: applications for the physician. Curr Opin Ophthalmol. (2018) 29:469–75. doi: 10.1097/ICU.0000000000000503
PubMed Abstract | Crossref Full Text | Google Scholar
8. Guntinas-Lichius O, Prengel J, Cohen O, Mäkitie AA, Vander Poorten V, Ronen O, et al. Pathogenesis, diagnosis and therapy of facial synkinesis: a systematic review and clinical practice recommendations by the international head and neck scientific group. Front Neurol. (2022) 13:1019554. doi: 10.3389/fneur.2022.1019554
PubMed Abstract | Crossref Full Text | Google Scholar
9. Ramey L, Osborne C, Kasitinon D, Juengst S. Apps and mobile health technology in rehabilitation: the good, the bad, and the unknown. Phys Med Rehabil Clin N Am. (2019) 30:485–97. doi: 10.1016/j.pmr.2018.12.001
PubMed Abstract | Crossref Full Text | Google Scholar
10. Dicianno BE, Parmanto B, Fairman AD, Crytzer TM, Yu DX, Pramana G, et al. Perspectives on the evolution of mobile (mHealth) technologies and application to rehabilitation. Phys Ther. (2015) 95(3):397–405. doi: 10.2522/ptj.20130534
PubMed Abstract | Crossref Full Text | Google Scholar
11. Ernsting C, Dombrowski SU, Oedekoven M, O’Sullivan JL, Kanzler E, Kuhlmey A, et al. Using smartphones and health apps to change and manage health behaviors: a population-based survey. J Med Internet Res. (2017) 19(4):e101. doi: 10.2196/jmir.6838
PubMed Abstract | Crossref Full Text | Google Scholar
12. Szczepura A, Holliday N, Neville C, Johnson K, Khan Khan AJ, Oxford SW, et al. Raising the digital profile of facial palsy: national surveys of patients’ and clinicians’ experiences of changing UK treatment pathways and views on the future role of digital technology. J Med Internet Res. (2020) 22(10):e20406. doi: 10.2196/20406
PubMed Abstract | Crossref Full Text | Google Scholar
13. Sanches EE, de Jongh FW, Ingels KJAO, Pouwels S. e-Health and telemedicine implementation in facial paralysis: challenges and pitfalls. Eur J Plast Surg. (2021) 44:429–34. doi: 10.1007/s00238-021-01802-8
PubMed Abstract | Crossref Full Text | Google Scholar
14. Taeger J, Bischoff S, Hagen R, Rak K. Utilization of smartphone depth mapping cameras for app-based grading of facial movement disorders: development and feasibility study. JMIR Mhealth Uhealth. (2021) 9(1):e19346. doi: 10.2196/19346
PubMed Abstract | Crossref Full Text | Google Scholar
16. Zhou L, Bao J, Setiawan IMA, Saptono A, Parmanto B. The mhealth app usability questionnaire (MAUQ): development and validation study. JMIR Mhealth Uhealth. (2019) 7(4):e11500. doi: 10.2196/11500
PubMed Abstract | Crossref Full Text | Google Scholar
17. Maramba I, Chatterjee A, Newman C. Methods of usability testing in the development of eHealth applications: a scoping review. Int J Med Inf. (2019) 126:95–104. doi: 10.1016/j.ijmedinf.2019.03.018
PubMed Abstract | Crossref Full Text | Google Scholar
18. Moshagen M, Thielsch MT. Facets of visual aesthetics. Int J Hum Comput Stud. (2010) 68(10):689–709. doi: 10.1016/j.ijhcs.2010.05.006
Crossref Full Text | Google Scholar
19. Kortum PT, Bangor A. Usability ratings for everyday products measured with the system usability scale. Int J Hum Comput Interact. (2013) 29(2):67–76. doi: 10.1080/10447318.2012.681221
Crossref Full Text | Google Scholar
21. Sánchez Rodríguez MT, Collado Vázquez S, Martín Casas P, Cano de la Cuerda R. Neurorehabilitation and apps: a systematic review of mobile applications. Neurologia (Engl Ed). 2018. 33 p. 313–26. doi: 10.1016/j.nrl.2015.10.005
PubMed Abstract | Crossref Full Text | Google Scholar
22. Lunde P, Bye A, Bruusgaard KA, Hellem E, Nilsson BB. Patients’ experiences of using a smartphone app after cardiac rehabilitation: qualitative study. JMIR Hum Factors. (2022) 9(1):e34294. doi: 10.2196/34294
PubMed Abstract | Crossref Full Text | Google Scholar
23. Liu T, Xie S, Wang Y, Tang J, He X, Yan T, et al. Effects of app-based transitional care on the self-efficacy and quality of life of patients with spinal cord injury in China: randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9(4):e22960. doi: 10.2196/22960
PubMed Abstract | Crossref Full Text | Google Scholar
24. Hellström K, Lindmark B, Wahlberg B, Fugl-Meyer AR. Self-efficacy in relation to impairments and activities of daily living disability in elderly patients with stroke: a prospective investigation. J Rehabil Med. (2003) 35(5):202–7. doi: 10.1080/16501970310000836
PubMed Abstract | Crossref Full Text | Google Scholar
25. Bailey R. Examining daily physical activity in community-dwelling adults with stroke using social cognitive theory: an exploratory, qualitative study. Disabil Rehabil. (2020) 42(18):2631–9. doi: 10.1080/09638288.2019.1568591
PubMed Abstract | Crossref Full Text | Google Scholar
26. Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Hum Comput Interact. (2008) 24(6):574–94. doi: 10.1080/10447310802205776
Crossref Full Text | Google Scholar
28. Machetanz K, Oberle L, Wang SS, Weinbrenner E, Gorbachuk M, Lauer H, et al. Outpatient care for facial palsy—a survey on patient satisfaction in uni- and interdisciplinary approaches. Front Neurol. (2024) 15:1354583. doi: 10.3389/fneur.2024.1354583
PubMed Abstract | Crossref Full Text | Google Scholar
31. Hawley-Hague H, Tacconi C, Mellone S, Martinez E, Ford C, Chiari L, et al. Smartphone apps to support falls rehabilitation exercise: app development and usability and acceptability study. JMIR Mhealth Uhealth. (2020) 8(9):e15460. doi: 10.2196/15460
PubMed Abstract | Crossref Full Text | Google Scholar
32. Moral-Munoz JA, Zhang W, Cobo MJ, Herrera-Viedma E, Kaber DB. Smartphone-based systems for physical rehabilitation applications: a systematic review. Assist Technol. (2021):223–36. doi: 10.1080/10400435.2019.1611676
PubMed Abstract | Crossref Full Text | Google Scholar
33. Cucciniello M, Petracca F, Ciani O, Tarricone R. Development features and study characteristics of mobile health apps in the management of chronic conditions: a systematic review of randomised trials. NPJ Dig Med. (2021) 4(1):144. doi: 10.1038/s41746-021-00517-1
PubMed Abstract | Crossref Full Text | Google Scholar
34. Richardson J, Letts L, Sinclair S, Chan D, Miller J, Donnelly C, et al. Using a web-based app to deliver rehabilitation strategies to persons with chronic conditions: development and usability study. JMIR Rehabil Assist Technol. (2021) 8(1):e19519. doi: 10.2196/19519
PubMed Abstract | Crossref Full Text | Google Scholar
35. Schroeder T, Haug M, Gewald H. Data privacy concerns using mHealth apps and smart speakers: comparative interview study among mature adults. JMIR Form Res. (2022) 6(6):e28025. doi: 10.2196/28025
PubMed Abstract | Crossref Full Text | Google Scholar
36. Prasad A, Sorber J, Stablein T, Anthony D, Kotz D. Understanding sharing preferences and behavior for mhealth devices. Proceedings of the ACM Conference on Computer and Communications Security New York, NY, USA: ACM (2012). p. 117–28. doi: 10.1145/2381966.2381983
Crossref Full Text
37. Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom clinical research network database. BMC Med Res Methodol. (2013) 13(1):104. doi: 10.1186/1471-2288-13-104
PubMed Abstract | Crossref Full Text | Google Scholar
38. Tullis TS, Stetson JN. A comparison of questionnaires for assessing website usability ABSTRACT: introduction. Usability Professional Association Conference (2004). p. 1–12
39. Fattah AY, Gurusinghe ADR, Gavilan J, Hadlock TA, Marcus JR, Marres H, et al. Facial nerve grading instruments: systematic review of the literature and suggestion for uniformity. Plast Reconstr Surg. (2015) 135(2):569–79. doi: 10.1097/PRS.0000000000000905
PubMed Abstract | Crossref Full Text | Google Scholar
40. Banks CA, Bhama PK, Park J, Hadlock CR, Hadlock TA. Clinician-graded electronic facial paralysis assessment: the eFACE. Plast Reconstr Surg. (2015) 136(2):223e–30e. doi: 10.1097/PRS.0000000000001447
PubMed Abstract | Crossref Full Text | Google Scholar
41. Miller MQ, Hadlock TA, Fortier E, Guarin DL. The auto-eFACE: machine learning–enhanced program yields automated facial palsy assessment tool. Plast Reconstr Surg. (2021) 147(2):467–74. doi: 10.1097/PRS.0000000000007572
PubMed Abstract | Crossref Full Text | Google Scholar
link







