A randomized controlled trial of a digital lifestyle intervention involving postoperative patients with colorectal cancer
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Google Scholar
Sauer, R. et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N. Engl. J. Med. 351, 1731–1740 (2004).
Google Scholar
Heald, R. J. & Ryall, R. D. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1, 1479–1482 (1986).
Google Scholar
Kapiteijn, E. et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N. Engl. J. Med. 345, 638–646 (2001).
Google Scholar
Park, I. J. & Kim, J. C. Intersphincteric resection for patients with low-lying rectal cancer: Oncological and functional outcomes. Ann. Coloproctol. 34, 167–174 (2018).
Google Scholar
Lim, S. L. et al. Risk factors associated with low anterior resection syndrome: A cross-sectional study. Ann. Coloproctol. 39, 427–434 (2023).
Google Scholar
Meyerhardt, J. A. et al. Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: Findings from CALGB 89803. J. Clin. Oncol. 24, 3535–3541 (2006).
Google Scholar
Morales-Oyarvide, V. et al. Dietary insulin load and cancer recurrence and survival in patients with Stage III colon cancer: Findings from CALGB 89803 (alliance). J. Natl. Cancer Inst. 111, 170–179 (2019).
Google Scholar
Wu, J. et al. Multimodal prerehabilitation for elderly patients with sarcopenia in colorectal surgery. Ann. Coloproctol. 40, 3–12 (2024).
Google Scholar
Kahi, C. J. et al. Colonoscopy surveillance after colorectal cancer resection: Recommendations of the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 150, 758–768.e711 (2016).
Google Scholar
Yang, S. et al. Development of a home health care service platform for ostomy patient management. Ann. Coloproctol. 40, 36–43 (2024).
Google Scholar
Chung, I. Y. et al. An assessment of physical activity data collected via a smartphone app and a smart band in breast cancer survivors: Observational study. J. Med Internet Res. 21, 13463 (2019).
Google Scholar
Rocamora González, C. et al. Mindfulness based intervention through mobile app for colorectal cancer people awaiting surgery: A randomized clinical trial. Cir. Esp. (Engl. Ed. 100, 747–754 (2022)..
Salmani, H., Nahvijou, A. & Sheikhtaheri, A. Smartphone-based application for self-management of patients with colorectal cancer: Development and usability evaluation. Support Care Cancer 30, 3249–3258 (2022).
Google Scholar
Ayyoubzadeh, S. M., Shirkhoda, M., Kalhori, S. R. N., Mohammadzadeh, N. & Zakerabasali, S. A smartphone remote monitoring app to follow up colorectal cancer survivors: Requirement analysis. JMIR Cancer 8, e18083 (2022).
Google Scholar
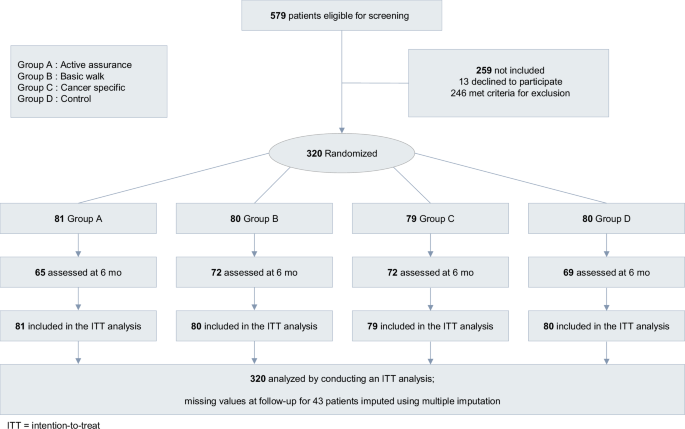
Kim, Y. I. et al. Lifestyle interventions after colorectal cancer surgery using a mobile digital device: A study protocol for a randomized controlled trial. Med. (Baltim.) 101, e31264 (2022).
Google Scholar
Laing, B. Y. et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: A randomized, controlled trial. Ann. Intern Med. 161, S5–S12 (2014).
Google Scholar
Nord, A., Svensson, L., Hult, H., Kreitz-Sandberg, S. & Nilsson, L. Effect of mobile application-based versus DVD-based CPR training on students’ practical CPR skills and willingness to act: A cluster randomised study. BMJ Open 6, e010717 (2016).
Google Scholar
Tighe, J. et al. Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: A pilot randomised controlled trial. BMJ Open 7, e013518 (2017).
Google Scholar
Bertoni, S. et al. Digital postoperative follow-up after colorectal resection: A multi-center preliminary qualitative study on a patient reporting and monitoring application. Update Surg. 76, 139–146 (2024).
Google Scholar
Kupper, B. E. C. et al. Developing and validation of a smartphone app for post-discharge early follow-up after colorectal cancer surgeries. Digit Health 10, 20552076241292389 (2024).
Google Scholar
Liao, Y. T. et al. Wearable mobile health device for monitoring postoperative ambulation among patients with colorectal cancer undergoing minimally invasive surgery: A prospective comparison study. Int. J. Med. Robot 20, e2626 (2024).
Google Scholar
Free, C. et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLOS Med. 10, e1001363 (2013).
Google Scholar
Kitsiou, S., Paré, G., Jaana, M. & Gerber, B. Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLOS One 12, e0173160 (2017).
Google Scholar
Moy, M. L. et al. Long-term effects of an Internet-mediated pedometer-based walking program for chronic obstructive pulmonary disease: Randomized controlled trial. J. Med. Internet Res. 18, e215 (2016).
Google Scholar
Chung, I. Y. et al. Exercise promotion and distress reduction using a mobile app-based community in breast cancer survivors. Front Oncol. 9, 1505 (2020).
Google Scholar
Park, Y. R. et al. Managing patient-generated health data through mobile personal health records: Analysis of usage data. JMIR MHealth UHealth 6, e89 (2018).
Google Scholar
Lillo-García, C. et al. Prehabilitation through a mobile application (PREHAPP) in major colon cancer surgery. Br. J. Surg. 110, (2023).
Jakob, R. et al. Factors influencing adherence to mHealth apps for prevention or management of noncommunicable diseases: Systematic review. J. Med. Internet Res. 24, e35371 (2022).
Google Scholar
Arnhold, M., Quade, M. & Kirch, W. Mobile applications for diabetics: A systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J. Med. Internet Res. 16, e104 (2014).
Google Scholar
Chin, S. O. et al. Successful weight reduction and maintenance by using a smartphone application in those with overweight and obesity. Sci. Rep. 6, 34563 (2016).
Google Scholar
May, C. N. et al. Weight loss maintenance after a digital commercial behavior change program (Noom Weight): Observational cross-sectional survey study. Obes. Sci. Pract. 9, 443–451 (2023).
Google Scholar
Giebel, G. D. et al. Problems and barriers related to the use of digital health applications: Scoping review. J. Med. Internet Res. 25, e43808 (2023).
Google Scholar
Hernandez, G. et al. EuroQol (EQ-5D-5L) validity in assessing the quality of life in adults with asthma: Cross-sectional study. J. Med. Internet Res. 21, e10178 (2019).
Google Scholar
Tran, B. T. et al. Measurement of health-related quality of life among colorectal cancer patients using the Vietnamese value set of the EQ-5D-5L. Patient Prefer Adherence 14, 2427–2437 (2020).
Google Scholar
Brazier, J. E., Rowen, D., Lloyd, A. & Karimi, M. Future directions in valuing benefits for estimating QALYs: Is time up for the EQ-5D?. Value Health 22, 62–68 (2019).
Google Scholar
Efthymiadou, O., Mossman, J. & Kanavos, P. Health related quality of life aspects not captured by EQ-5D-5L: Results from an international survey of patients. Health Policy 123, 159–165 (2019).
Google Scholar
The Italian ColoRectal Anastomotic Leakage (iCral3) Study Group Patient-reported outcomes and return to intended oncologic therapy after colorectal enhanced recovery pathway: The iCral3 prospective study. Ann. Surg. Open 4, e267 (2023).
Google Scholar
Loria, A. & Fleming, F. J. Restoration of quality of life and functional recovery after colorectal cancer surgery in older adults. J. Clin. Oncol. 41, 5225–5227 (2023).
Google Scholar
Gielen, A. H. C. et al. Impact of anastomotic leakage after colorectal cancer surgery on quality of life: A systematic review. Dis. Colon Rectum 68, 154–170 (2025).
Google Scholar
Pieniowski, E. H. A. et al. Prevalence of low anterior resection syndrome and impact on quality of life after rectal cancer surgery: Population-based study. BJS Open 4, 935–942 (2020).
Google Scholar
Oliveira, M. R. et al. Covid-19 and the impact on the physical activity level of elderly people: A systematic review. Exp. Gerontol. 159, 111675 (2022).
Google Scholar
Lee, Y., Baek, S. & Shin, J. Changes in physical activity compared to the situation before the outbreak of COVID-19 in Korea. Int J. Environ. Res. Public Health 19, 126 (2021).
Google Scholar
Kameyama, H. et al. Quality of life of patients after colorectal cancer surgery as assessed using EQ-5D-5L scores]. Gan Kagaku Ryoho 44, 1083–1085 (2017).
Moher, D. et al. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J. Clin. Epidemiol. 63, e1–e37 (2010).
Google Scholar
Takano, E. et al. User experience of older people while using digital health technologies: A systematic review. Appl. Sci. 13, 12815 (2023).
Google Scholar
Reid, M. et al. Factors influencing seniors’ anxiety in using ICT. Soc. Sci. 13, 496 (2024).
Google Scholar
Rabin, R. & de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med 33, 337–343 (2001).
Google Scholar
Kim, J., Lee, H. J. & Jo, M. W. Health-related quality of life instrument with 8 items for use in patients with type 2 diabetes mellitus: A validation study in Korea. J. Prev. Med. Public Health 55, 234–242 (2022).
Google Scholar
Busija, L. et al. Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF-6D), Health Utilities Index Mark 3 (HUI3), Quality of Well-Being Scale (QWB), and Assessment of Quality of Life (AQoL). Arthritis Care Res (Hoboken) 63, S383–S412 (2011).
Google Scholar
Ward, W. L. et al. Reliability and validity of the functional assessment of cancer therapy-colorectal (FACT-C) quality of life instrument. Qual. Life Res. 8, 181–195 (1999).
Google Scholar
Ha, J. et al. Development of a fully automatic deep learning system for L3 selection and body composition assessment on computed tomography. Sci. Rep. 11, 21656 (2021).
Google Scholar
Clavien, P. A. et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 250, 187–196 (2009).
Google Scholar
Tsiplova, K., Pullenayegum, E., Cooke, T. & Xie, F. EQ-5D-derived health utilities and minimally important differences for chronic health conditions: 2011 Commonwealth Fund Survey of Sicker Adults in Canada. Qual. Life Res. 25, 3009–3016 (2016).
Google Scholar
Walters, S. J. & Brazier, J. E. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual. Life Res. 14, 1523–1532 (2005).
Google Scholar
Yu, J. et al. Uneven recovery patterns of compromised health-related quality of life (EQ-5D-3 L) domains for breast Cancer survivors: A comparative study. Health Qual. Life Outcomes 16, 143 (2018).
Google Scholar
link