Impact of pharmacist led mobile application on medication adherence and efficacy in chronic kidney disease
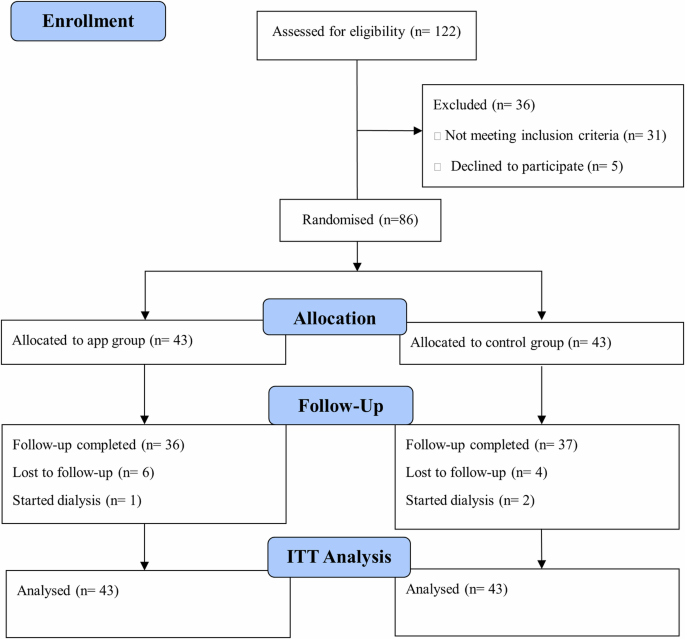
Kidney Health app was introduced in the current single centered RCT to patients with CKD, stages 3–5 in the intervention group, providing them with features as medications recording, personalized daily alarms and response recording, educational material and notification, data logging of labs and symptoms, and sending questions to the pharmacist while the control group received the standard of care. Patients were followed up by the pharmacist for 3 months and their medication adherence, clinical outcomes as well as app usability were assessed. The app group showed significant improvement in medication adherence, probability of becoming adherent and in some clinical outcomes such as eGFR and RBG compared to the control group. To our knowledge this is the first RCT to assess the impact of pharmacist-led mobile app intervention on medication adherence and efficacy in patients with CKD stages 3–5.
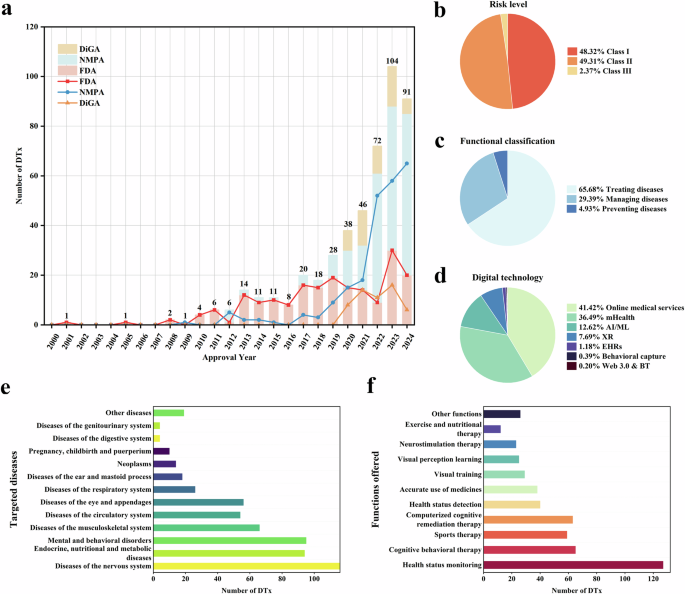
mHealth interventions have been investigated previously in different chronic diseases showing efficacy and positive impact on medication adherence27,28,29,30. In a recent meta-analysis that included 14 RCTs, mobile applications were associated with significant improvement in medication adherence in adults with chronic diseases. The main features of the apps included in the analysis were documentation, medication reminder, data sharing, feedback message, clinical decision support and education30. In a 3 months study, Mira et al. assessed medication adherence, errors and clinical outcomes after introducing an mHealth intervention offering reminders and medication education to chronically ill elderly patients. Patients in the app obtained significantly higher adherence scores, fewer errors and missed doses compared to the control group, adding to the evidence of the positive impact of such interventions27.
Previous studies carried out in the CKD population included mHealth interventions such as lifestyle advice and real time communication with nurses, education by nephrologist and mHealth technologies as well as diet and exercise follow-up and education31,32,33. Two studies includes apps with multiple features of data recording, education, communication channel and only one of them included reminders34,35. All studies showed significant improvement in some of the measures outcomes. These outcomes included knowledge and self-management scores, survival analysis and some clinical outcomes like blood pressure and eGFR.
Our study is one of the few RCTs done to evaluate the impact of an mHealth intervention on pre-dialysis patients with CKD. Liu et al. and Tsai et al. had similar intervention and population; however, they were retrospective and prospective cohort studies respectively, with different outcomes measured not focusing on medication adherence and its importance in such population31,34. RCTs were carried out by Sarker et al., Li et al., and Maneesri et al. on similar population however, medication adherence was not reported, and there were conflicting clinical outcomes results. Moreover, the type of mHealth intervention widely varied mainly focusing on education and lifestyle management, besides none of them mentioned a pilot phase for the mHealth intervention used32,33,35. In the current study we attempted to overcome previous studies’ limitations by adding a pilot phase, measuring medication adherence by two methods and using a more adaptable mHealth intervention while implementing a pharmacist-led approach.
Pharmacist-led digital interventions have demonstrated noticeably positive impact on medication adherence and clinical outcomes in patients with complex diseases and medication management29,36,37,38. Our study involved a pharmacist-led intervention thus having an added advantage compared to self-management or other healthcare professional-led interventions as the pharmacist had direct and active involvement with the patients through training the patients, carrying out personalized monthly follow-up interviews, immediate response to app-submitted questions and careful assessment of medication adherence.
Pharmacist-led studies in transplant, hypertension and diabetes populations have shown similar benefits as the current study, nevertheless our study is the first to confirm these effects in CKD population through using robust adherence measures and an mHealth platform29,37,38. A study that investigated the efficacy of a pharmacist-led mobile application on medication adherence and diabetes-related outcomes among women with gestational diabetes and followed up for 12 months post-partum, found the involvement of a pharmacist, reduced patients’ medication suspicion and provided encouragement for raising their medication adherence29. The pharmacist-led intervention used, significantly enhanced medication adherence and improved glycemic control compared to usual care group. Another study that examined the efficacy of improving medication safety through a pharmacist-led medication therapy monitoring and management app in post-transplant patients showed that such intervention helped develop a partnership between patients and clinicians as well as mitigate patient safety issues37.
Having a pilot phase is another one of the current study’s strengths. In the study carried by Mira et al., the authors emphasized the importance of carrying out a pilot phase as it allowed the app to be more adaptable to patients’ requirements and more acceptable to them as well as to healthcare professionals27. Thus, the pilot phase allowed Kidney Health app design to be based on the views and preferences of the target patients and the experience of healthcare professional along with assessing the usability during the app development.
Medication adherence is crucial in this unique population. Medication adherence was measured using SMAQ questionnaire as well as app reminders response. SMAQ was chosen as it was found to be a valid and reliable scale as well as being simple, short with good psychometric properties39,40. The baseline SMAQ measured percentage adherent was low in both groups (9.3–12.2%), when compared to previously mentioned estimates of adherence in CKD patients10.
This study analyses demonstrated sustained improvements in adherence and some clinical outcomes that are not solely attributable to time effects or the standard care. We reported a significantly higher percentage of adherent patients in the app group compared to the control group. This is in concordance with previous results reported by Mira et al. and Khah et al., where mHealth interventions with either reminders or education materials in chronically ill elderly patients or hemodialysis patients respectively, were used and medication adherence significantly improved after 3 months follow-up27,41. In the current study the increase in adherence in the app group was evident from the first follow-up and significantly higher than the baseline throughout the study period. While, in the control group it became evident by follow-up 2 hence having a higher median time of becoming adherent as shown by the Kaplan-Meier analysis. Even though adherence was higher in the app group compared to the control throughout the study reaching significance at follow-up 2 and 3, both groups showed significant increase at the end of the study. Anglada et al. assessed medication adherence in a single arm study of chronically ill patients, where an app for medication recording and reminders was introduced, they discussed the Hawthorne effect where patients improve an aspect of their behavior as medication adherence in response to awareness of being observed28. This might be a possible explanation for the significant increase in adherence in the control group, especially that our study had a higher frequency, monthly, follow-up. Still, despite this possibility the app group have shown a significant improvement in medication adherence compared to the control group.
Adherence reported through the app, percentage of alarms responded to, has shown significant positive correlation starting from follow-up 2 with SMAQ measured adherence. This positive correlation shows promising potential, firstly as previous studies did not estimate adherence as previously mentioned and secondly supports using mHealth recorded responses as a measure for medication adherence especially that there is no gold standard for measuring adherence.
As for the clinical outcomes in this study, they were used as surrogates for assessing medication efficacy and by measuring and reporting the within group changes, we were able to detect significant improvements in the app group patients’ eGFR and RBG. Few studies reported the impact of an mHealth intervention on kidney functions, and they did not report the within group changes significance. Li et al., reported a significantly higher eGFR in the app group, who had access to app with diet and exercise recording and education, compared to control group at the end of the 3 months study33. While, similar to our study Sarker et al., showed no significant changes in kidney function between the app group, who received education by nephrologist along with mHealth technology interventions, and the control group at the end of the study32. In the current study, significant difference was found in the interaction of app × time for eGFR, also by the end of the study, the app group had higher eGFR compared to control but it did not reach significance between groups. One possible explanation for the improvement in eGFR in both groups, is that the significant increase in adherence within both groups in the current study might have helped in slowing the disease progression, as adherence correlates to slower disease progression4.
The observed changes in the eGFR and RBG in the Kidney Health app group show potential for the usefulness of such intervention in improving medication efficacy and clinical outcomes in patients with CKD, through increasing medication adherence, providing educational material and a communication channel between patients and Pharmacists. Furthermore, features such as recording lab results and providing trend charts are all potential factors that might have helped as well.
To our knowledge previous studies with CKD-oriented apps did not assess usability. Assessing app usability is important as it can dictate the adoption of such interventions, users’ willingness to use them, sustained engagement as well as their actual usefulness and clinical impact42,43. Therefore, usability measured in the current study reflected the patients’ experience and willingness to use the app. We used the 10 question Arabic SUS, which is considered a well-designed, balanced questionnaire consisting of 5 questions with positive statements and 5 questions with negative statements. It has become a common method for measuring the usability for different digital products including digital health applications42.
Kidney health app had an above-average ASUS mean score throughout the follow-up period as well as a significant increase in the percentile of patients giving the app a score greater than 68 at the end of the study. Even though our app showed good usability and an increasing interaction with the app alarms over the follow-up period, most patients responded to less than 25% of the alarms and app features requiring data entry as lab tests, side effects, and sending questions had relatively low interaction. There may be several reasons for these results, patients might have found it extra work, moreover, being used to other channels of contact with the healthcare professionals leading to low interaction28. Also some of the app features needed internet connection (e.g. sending a question or data recording), so they will not function properly if there is an internet connection problem.
Despite the strengths of our study being an RCT with a pilot phase, one of the study limitations was being single centered. Also, as it was not feasible to provide patients with smart phones, patients had to own a smartphone to be recruited so they were more likely to be willing to try and use this type of intervention. Furthermore, patients provided their own laboratory data, as the study was carried out in a private nephrology clinic, so it was not feasible to withdraw samples. Another limitation was that we could not be sure that patients took the medications, however a well-accepted and validated medication adherence measurement tool was used along with adherence reported through the app. Moreover, when evaluating the relationship between both measures of medication adherence in the app group, they showed good correlation.
In conclusion, our study demonstrated how a pharmacist-led mHealth intervention succeeded in encouraging patients to adhere to their medication regimens through its multiple integrated features, thus showing the potential of such adherence aids in practice and on wider scale to help patients with CKD to be more self-dependent with the guidance of healthcare professionals such as the pharmacists to improve their medication adherence and efficacy.
link