Optimizing recovery after reverse shoulder arthroplasty with a personalised mobile health application compared to generic digital information: a protocol of a multicentre randomised controlled trial | BMC Musculoskeletal Disorders
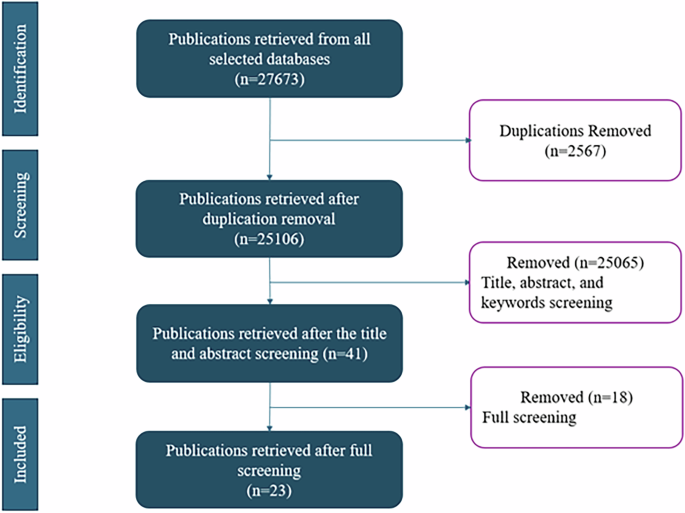
This study is a multicentre, single-blinded (assessor), two-armed, parallel-group RCT designed to evaluate the effectiveness of an interactive mHealth application compared to generic non-personalised digital information (non-interactive app) in the rehabilitation period of patients undergoing RSA: TRAPP (Treatment Reverse shoulder with APP) study. Two non-academic hospitals in the Netherlands will participate initially, with plans to include more based on the inclusion rate. Patients will be recruited from the orthopaedic outpatient clinic of these hospitals. Patients who are included in the study are randomised in a 1:1 ratio to either the intervention group or the control group. The study design is summarised in Fig. 1. The inclusion duration is expected to last 18 months, the total study duration is expected to last 40 months. This study is approved by the Institutional Review Board (METC Maxima Medical Centre, Eindhoven-Veldhoven, the Netherlands, IRB Nr. N22.075) and is registered in ClinicalTrials.gov (NCT06520085) on the 22nd of July 2024. Deviations to the protocol will be reported in ClinicalTrials.gov. This protocol is reported in accordance with the SPIRIT statement.
Participant selection
All patients scheduled for elective, primary RSA with degenerative disorders (such as shoulder osteoarthritis, rotator cuff arthropathy, or avascular necrosis) of the shoulder are eligible for this study. Patients are excluded from participation if they: 1) do not own or are not able to operate a smart device; 2) are scheduled for revision surgery; 3) have a proximal humerus fracture as primary diagnosis; 4) need an additional muscle transfer to be performed (latissimus dorsi/ teres major); 5) are unable to read and understand the Dutch language; 6) are unwilling to be randomized.
Surgery
Surgery is performed in a beach chair position using the deltopectoral approach. To access the glenohumoral joint a subscapularis tenotomy is performed. The Comprehensive Total Shoulder (Zimmer Biomet, Warsaw, Indiana, USA) or the Universe Reverse (Arthrex Inc, Munchen, Germany) is used. To correct retroversion or inclination on indication bone grafts are used to augment the glenoid. The subscapularis tendon will not be repaired.
Informed consent
Patients eligible for inclusion will be informed about the study by their treating physician and receive the patient information letter and the informed consent form. The patient is invited for an informative (telephone) meeting with a research nurse or researcher approximately one week after receiving the information. During this (telephone) meeting, the patient will be informed on the standard RSA procedure. Additionally, the patient will be informed about the study aim and procedures. After ensuring the patient has understood the information and after checking the in- and exclusion criteria, the patient will be asked to sign the informed consent form after agreement on participation. The patient will receive one of the fully signed copies of the patient information letter and one fully signed copy will be stored by the research institution.
Control group
The control group will receive postoperative information and a rehabilitation program via the non-interactive application, which is current standard care in both clinics. Information includes written information on the procedure, preparation, postoperative recovery and possible complications. Videos of the clinical team explaining use of the app, use of the sling, complications, wound care, pain treatment and physiotherapy exercises are available at set time intervals. The application will use the date of surgery to assure the timing of information is timely. Patients will receive alerts about information being available in the app with the use of push notifications. In the first three weeks the patient will receive information about the rehabilitation exercise program. The patients get push notification with exercising videos aimed at optimizing hand, wrist and elbow functioning. For the shoulder pendulum exercises are advised. After three weeks these exercises are aimed to optimize the shoulder function. Patients are advised to use their sling for the first 2 weeks if necessary. Patients will receive inpatient physiotherapy every day until discharge, starting from the day of surgery. All patients are instructed to start with physiotherapy when discharged. The patient is responsible for contacting the outpatient physiotherapist. Pain scores are measured regularly using the Numeric Rating Scale (NRS) [8].
Intervention group
The intervention group receives the same care as the control group, including access to postoperative physiotherapy. Only the app is different in that it provides interactive and personalized information and a personalized rehabilitation program. Both the timing and the amount and nature of the exercises are personalized.
The content of the interactive information in the mHealth application was developed after a review of the literature on postoperative rehabilitation following RSA, Dutch RSA rehabilitation protocol of the National Shoulder Network, and patient interviews. Five patients who underwent RSA according to usual care were interviewed on their experiences about application usage. During this interview patients were asked about their experience with information provision (via the non-interactive application) after their procedure, what type of information they missed and how information provision could be improved. In general patients missed information about the daily exercises, they missed a final endpoint of the application, and one patient missed a structured overview of the information.
Personalized rehabilitation program
Two interdisciplinary consensus meetings with an orthopaedic surgeon, ten expert shoulder physiotherapists and two researchers were organised. The goal of these meetings was to create a consensus-based exercise protocol based on existing literature, rehabilitation protocols and expert opinion of specialised shoulder-physiotherapists. In the second consensus meeting participants discussed the feasibility of the exercise protocol. They agreed that exercising twice a day (preferably morning and evening) is optimal.
The rehabilitation protocol was based on three recent studies. Kornuijt et al. published the results of a cohort study in which 100 patients were treated with direct active mobilisation starting the first day post-surgery [2]. Conclusion of this study was that early mobilisation is safe, only 5 (5.0%) out of 17 complications were categorised as potentially related to early mobilisation (prolonged pain n = 3, dislocation n = 1, acromial stress fracture n = 1). In a RCT comparing delayed versus early rehabilitation, for both protocols good outcomes were reported. However, no additional benefit of one rehabilitation strategy over another was found [9]. In this study 2 weeks post-surgery the shoulder was passively and actively-assisted mobilised. After 6 weeks the exercises progressed to active movement. This protocol is not comparable to Kornuijt et al. in terms of early mobilisation. In a study of Lee et al. 6 weeks of immobilisation was compared to 3 weeks of immobilisation and to direct mobilisation [10]. For both accelerated rehabilitation protocols non inferiority compared to 6 weeks of immobilisation was confirmed.
Based on the exercise protocols presented in literature, patient interviews and expert opinions a consensus based exercise protocol was created. The exercise protocol was divided in 5 different exercise categories based on muscle group and/or function: 1) elbow, wrist and hand; 2) spine; 3) scapula; 4) glenohumeral movement and; 5) shoulder rotation. In these categories exercises were divided into (maximum) five phases ranging from 1 to 5, in which the difficulty of the exercises increased with each phase according to exercise physiology principles [11]. From closed chain to gradually more open and from unloaded to loaded exercises [12]. The exercise protocol is shown in Table 1. All patients start in phase 1 and progress at their own pace. Each patient is stimulated to practice twice a day for at least 15 min, by prompts from the app. They will receive push notifications to prompt exercising once in the morning and once in the afternoon on set times chosen by the patient. Patients can progress in exercise difficulty if their pain level is acceptable during the exercise, measured on a 4 point likert scale (severe pain– moderate pain– mild pain – no pain). They can proceed to the next exercise if they have a Likert scale score of mild or no pain on two consecutive days. To prevent patients progress too quickly through the exercise protocol, we integrated a safety system. This means that specific exercises are only released after a certain period of time has elapsed, as can been seen in the exercise protocol (Table 1). When patients do not proceed to the next level the research nurse and treating physician will be notified of the stagnant recovery.
Interactive and personalized information
Patients in the intervention group have the opportunity to upload photographs of their wound in the application to monitor wound healing, three days postoperatively. These photos are assessed by a nurse and discussed with the patient and treating physician in case abnormal wound healing is present. Patients have the option to ask questions via the application. When a question is submitted the clinical team will get a notification via email. Patients are informed that we aim to reply within 48 h on working days. If there are any alarm symptoms, such as wound leakage, fever, shivering or general malaise, patients will be informed to call the emergency department immediately.
Randomization and blinding
The application will randomise participants when downloading the application per centre (cluster randomisation) on a 1:1 ratio. In order to download the application the patient will receive a personal code via e-mail. After entering this code the application will randomly assign participants to either the intervention group or the control group. The control group will receive non-interactive standard information via a basic application. Questionnaires will be sent through the application for both groups.
Since the application relies on interaction between patient and clinical care team, both the patient and clinicians cannot be blinded. The researcher that will perform data analysis will be blinded to group allocation.
Outcome measures
Primary outcome
The primary outcome of this study will be postoperative functioning at 6 weeks, measured using the OSS [13]. The OSS measures shoulder function and pain using 12 questions from which a sum score is calculated from 0 to 48. A lower score means more disability and pain. Patients will complete the OSS preoperatively and at six weeks. As a secondary outcome OSS will be completed as well at three months and one year postoperatively.
Secondary outcomes
Level of pain will be measured using the Numeric Rating Scale (NRS) [8]. In order to complete the NRS patients will be asked to rate the amount of pain experienced from the treated shoulder in the past week, both in rest and during activity, on a scale from 0–10 (a score 10 is indicating the worst pain imaginable). To evaluate the quality of life the EQ-5D-5L is used [14]. This is a patient-reported questionnaire that evaluates quality of life. Dutch normative values will be used to calculate sum scores (on a scale from 0–1, higher scores indicate better quality of life). The Disability of the Arm, Shoulder and Hand (DASH) questionnaire are used to measure shoulder function [15]. The DASH is a patient-reported questionnaire that evaluates functional limitations of the arm, shoulder and hand in daily activities. We will use the validated Dutch Language Version of the DASH score (on a scale from 0–100 score, higher score indicates better functioning). Satisfaction of the patient with the provided information is measured using a 5-point Likert scale. Active range of motion is measured by a research nurse or orthopaedic surgeon at the outpatient clinic. Abduction, anteflexion, and external rotation are measured with a goniometer, while internal rotation is classified using the Constant-Murley scoring method by recording the highest anatomic landmark the patient’s thumb was able to reach. The patient reported questionnaires will be sent through the application for both groups. All measures are collected preoperatively, at six weeks, three months and one year postoperatively.
At one year postoperative readmission rates and reasons will be evaluated. The reason for readmission and the timing after the operation will be documented. Complications such as nerve damage, infection, dislocation and thromboembolic event are also analysed at one year postoperatively. Complications are retrieved from the Electronic Medical Record (EMR) and are rated according to the Clavien-Dindo classification which consists of five grades with a definition of the severity of the complication [16].
After final follow up of all patients a process evaluation will be conducted on the use of the application. The individual usage time will be retrieved from the application and compared with the treatment response. The treatment adherence will be evaluated for each exercise.
Data management
All collected data will be de-identified and given a study code. Data will be stored on a secured server of the app provider only accessible to authorized personnel through a two-factor authentication protocol. Data will be stored for 15 years to facilitate monitoring of the study by authorities. No pre-planned trial auditing or Data monitoring Committee is needed for this study as this study is considered not applicable to the Dutch Medical Research Involving Human Subject Act.
Power calculation
An a priori power sample size calculation was performed using G*power software package defining our sample size of 170 [17]. A difference of 5.47 points in physical functioning is chosen to be clinically relevant difference between the two groups. This effect size was chosen based on previous comparable research on patients receiving an interactive app compared to standard care in total knee arthroplasty [7]. In this study the primary endpoint was function of the knee, measured on a comparable outcome scale as the OSS, ranging between 0–100. An alpha of 0.05 and beta of 0.2 was chosen which resulted in a minimal sample size of 146 (73 in each group). Taking into account a drop-out of 15.6%, based on previous research [7] resulted in a total number of 170 patients.
Data analysis
Baseline characteristics will be presented as mean and standard deviation (SD) for continuous variables or as median and inter quartile range, and number and percentages for categorical variables. Baseline characteristics will be stratified by group allocation. We will also describe the average use time of the app during the total study duration and the interaction time with the different exercises in the intervention group, as means and SD. Correlations between app usage time and interaction time with primary and secondary outcomes will be analysed in the intervention group, to check if this influenced results.
We will examine the data for missing values, depending on the type of missing data an adequate technique for handling the missing data will be chosen. Data will be imputed if > 5% is missing. In case data is imputed we will perform a sensitivity analysis using only complete cases.
An intention to treat analysis and a per protocol analysis will be performed to estimate the effectiveness. For evaluating the effectiveness on the primary and secondary outcomes between baseline and at each consecutive follow up scores we will use a linear mixed-effects regression model with a random intercept to account for the repeated measures within each patient. We will use a 3-level structure including a fixed effect for treatment and random effects for both centres and participants. Linear mixed-effects regression accounts for the dependency of repeated measurements within a participant. Transformation may be used when model assumptions, such as normality, are violated. The effectiveness between groups of outcomes measured at a single follow-up point – LoS and complications – will be evaluated using a two-sample t-test or Mann–Whitney U test in case of non-normal data. Package for the Social Sciences (SPSS) [18] and R [19] will be used to carry out the analysis. Effect sizes with 95% confidence intervals will be reported, together with a 2-sided P-value. A p-value of < 0.05 is viewed as statistically significant.
link