Predicting postprandial glucose excursions to personalize dietary interventions for type-2 diabetes management
Ahmad, E., Lim, S., Lamptey, R., Webb, D. R. & Davies, M. J. Type 2 diabetes. Lancet 400, 1803–1820 (2022).
Google Scholar
GBD 2021 Diabetes Collaborators. Global, regional, and National burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of disease study 2021. Lancet 402, 203–234 (2023).
Google Scholar
Chew, N. W. S. et al. The global burden of metabolic disease: data from 2000 to 2019. Cell. Metab. 35, 414–428e3 (2023).
Google Scholar
Borse, S. P., Chhipa, A. S., Sharma, V., Singh, D. P. & Nivsarkar, M. Management of type 2 diabetes: current strategies, unfocussed aspects, challenges, and alternatives. Med. Princ Pract. 30, 109–121 (2021).
Google Scholar
Umphonsathien, M. et al. Effects of intermittent very-low calorie diet on glycemic control and cardiovascular risk factors in obese patients with type 2 diabetes mellitus: A randomized controlled trial. J. Diabetes Invest. 13, 156–166 (2022).
Google Scholar
Sellahewa, L., Khan, C., Lakkunarajah, S. & Idris, I. A. Systematic Review of Evidence on the Use of Very Low Calorie Diets in People with Diabetes. (2017).
Bolla, A. M., Caretto, A., Laurenzi, A., Scavini, M. & Piemonti, L. Low-Carb and Ketogenic Diets in Type 1 and Type 2 Diabetes. Nutrients 11, (2019).
Low-glycemic index. Diets as an intervention for diabetes: a systematic review and meta-analysis. Am. J. Clin. Nutr. 110, 891–902 (2019).
Google Scholar
Al-Adwi, M. E. et al. Effects of different diets on glycemic control among patients with type 2 diabetes: A literature review. Nutr. Health. (2023).
Google Scholar
Systematic review and. meta-analysis of different dietary approaches to the management of type 2 diabetes. Am. J. Clin. Nutr. 97, 505–516 (2013).
Google Scholar
Ruijgrok, C. et al. Reducing postprandial glucose in dietary intervention studies and the magnitude of the effect on diabetes-related risk factors: a systematic review and meta-analysis. Eur. J. Nutr. 60, 259–273 (2020).
Google Scholar
Diabetes & Diagnosis & Tests. https://diabetes.org/about-diabetes/diagnosis
Antonio, C. Postprandial glucose regulation and diabetic complications. Arch. Intern. Med. 164, 2090–2095 (2004).
Google Scholar
Hershon, K. S., Hirsch, B. R. & Odugbesan, O. Importance of postprandial glucose in relation to A1C and cardiovascular disease. Clin. Diabetes. 37, 250–259 (2019).
Google Scholar
Post-prandial hyperglycemia. Is an important predictor of the incidence of diabetic microangiopathy in Japanese type 2 diabetic patients. Biochem. Biophys. Res. Commun. 336, 339–345 (2005).
Google Scholar
Bent, B. et al. Engineering digital biomarkers of interstitial glucose from noninvasive smartwatches. NPJ Digit. Med. 4, 89 (2021).
Google Scholar
Cox, D. J. et al. Behavioral strategies to lower postprandial glucose in those with type 2 diabetes May also lower risk of coronary heart disease. Diabetes Ther. 10, 277–281 (2019).
Google Scholar
Yao, J. et al. Diet, physical activity, and sleep in relation to postprandial glucose responses under free-living conditions: an intensive longitudinal observational study. Int. J. Behav. Nutr. Phys. Act. 21, 142 (2024).
Google Scholar
Leahy, J. J. L. et al. Optimizing postprandial glucose management in adults with Insulin-Requiring diabetes: report and recommendations. J. Endocr. Soc. 3, 1942–1957 (2019).
Google Scholar
Association of the. Glucose patterns after a single nonstandardized meal with the habitual diet composition and features of the daily glucose profile in individuals without diabetes. Am. J. Clin. Nutr. 121, 246–255 (2025).
Google Scholar
de Carvalho, G. B. et al. Effect of different dietary patterns on glycemic control in individuals with type 2 diabetes mellitus: A systematic review. Crit. Rev. Food Sci. Nutr. 60, 1999–2010 (2020).
Google Scholar
Hirsch, S., Barrera, G., Leiva, L., de la Maza, M. P. & Bunout, D. Variability of glycemic and insulin response to a standard meal, within and between healthy subjects. Nutr. Hosp. 28, 541–544 (2013).
Google Scholar
Zeevi, D. et al. Personalized nutrition by prediction of glycemic responses. Cell 163, 1079–1094 (2015).
Google Scholar
Pasmans, K., Meex, R. C. R., van Loon, L. J. C. & Blaak, E. E. Nutritional strategies to attenuate postprandial glycemic response. Obes Rev 23, e13486 (2022).
Gibney, E. R. Personalised nutrition – phenotypic and genetic variation in response to dietary intervention. Proceedings of the Nutrition Society 79, 236–245 (2020).
Brown, S. A. et al. Biobehavioral determinants of glycemic control in type 2 diabetes: A systematic review and meta-analysis. Patient Educ. Couns. 99, 1558–1567 (2016).
Google Scholar
Nelson, K. M., McFarland, L. & Reiber, G. Factors influencing disease Self-Management among veterans with diabetes and poor glycemic control. J. Gen. Intern. Med. 22, 442–447 (2007).
Google Scholar
Walker, R. J., Smalls, B. L., Hernandez-Tejada, M. A., Campbell, J. A. & Egede, L. E. Effect of diabetes self-efficacy on glycemic control, medication adherence, self-care behaviors, and quality of life in a predominantly low-income, minority population. Ethn. Dis. 24, 349 (2014).
Google Scholar
Hessler, D. et al. Reductions in regimen distress are associated with improved management and glycemic control over time. Diabetes Care. 37, 617–624 (2014).
Google Scholar
Berkowitz, S. A. et al. Food insecurity, food ‘deserts,’ and glycemic control in patients with diabetes: A longitudinal analysis. Diabetes Care. 41, 1188–1195 (2018).
Google Scholar
Rein, M. et al. Effects of personalized diets by prediction of glycemic responses on glycemic control and metabolic health in newly diagnosed T2DM: a randomized dietary intervention pilot trial. BMC Med. 20, 1–13 (2022).
Google Scholar
Bush, C. L. et al. Toward the definition of personalized nutrition: A proposal by the American nutrition association. J. Am. Coll. Nutr. 39, 5–15 (2020).
Google Scholar
Bermingham, K. M. et al. Effects of a personalized nutrition program on cardiometabolic health: a randomized controlled trial. Nat. Med. 30, 1888–1897 (2024).
Google Scholar
Arias-Marroquín, A. T. et al. Personalized versus Non-personalized nutritional recommendations/interventions for type 2 diabetes mellitus remission: A narrative review. Diabetes Ther. 15, 749–761 (2024).
Google Scholar
Huynh, P., Fleisch, E., Brändle, M., Kowatsch, T. & Jovanova, M. Digital health technologies for metabolic disorders in older adults: A scoping review protocol. BioRxiv (2024).
Google Scholar
Nahum-Shani, I. et al. Just-in-Time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann. Behav. Med. 52, 446–462 (2018).
Google Scholar
A Just-In-Time. Adaptive intervention (JITAI) for smoking cessation: feasibility and acceptability findings. Addict. Behav. 136, 107467 (2023).
Google Scholar
Vinci, C. et al. Proximal effects of a Just-in-Time adaptive intervention for smoking cessation with wearable sensors: microrandomized trial. JMIR Mhealth Uhealth. 13, e55379 (2025).
Google Scholar
Hardeman, W., Houghton, J., Lane, K., Jones, A. & Naughton, F. A systematic review of just-in-time adaptive interventions (JITAIs) to promote physical activity. Int. J. Behav. Nutr. Phys. Act. 16, 31 (2019).
Google Scholar
Daryabeygi-Khotbehsara, R. et al. Just-In-Time adaptive intervention to sit less and move more in people with type 2 diabetes: protocol for a microrandomized trial. JMIR Res. Protoc. 12, e41502 (2023).
Google Scholar
Zhao, L. et al. A micro-randomized pilot study to examine the impact of just-in-time nudging on after-dinner snacking in adults with type 2 diabetes: A study protocol. Diabetes Obes. Metab. 25, 2439–2446 (2023).
Google Scholar
Zhao, Q. et al. Chinese diabetes datasets for data-driven machine learning. Sci. Data. 10, 35 (2023).
Google Scholar
Annuzzi, G. et al. Impact of nutritional factors in blood glucose prediction in type 1 diabetes through machine learning. IEEE Access. 11, 17104–17115 (2023).
Google Scholar
Xiong, X., Xue, Y., Cai, Y., He, J. & Su, H. Prediction of personalised postprandial glycaemic response in type 1 diabetes mellitus. Front. Endocrinol. 15, 1423303 (2024).
Google Scholar
Darby, A., Strum, M. W., Holmes, E. & Gatwood, J. A. Review of nutritional tracking mobile applications for diabetes patient use. Diabetes Technol. Ther. 18, 200–212 (2016).
Google Scholar
Corsica, J. A. et al. Mobile apps for diabetes self-management: an updated review of app features and effectiveness. J. Behav. Med. 48, 137–148 (2025).
Google Scholar
Krukowski, R. A., Harvey, J., Borden, J., Stansbury, M. L. & West, D. S. Expert opinions on reducing dietary self-monitoring burden and maintaining efficacy in weight loss programs: A Delphi study. Obes. Sci. Pract. 8, 401–410 (2022).
Google Scholar
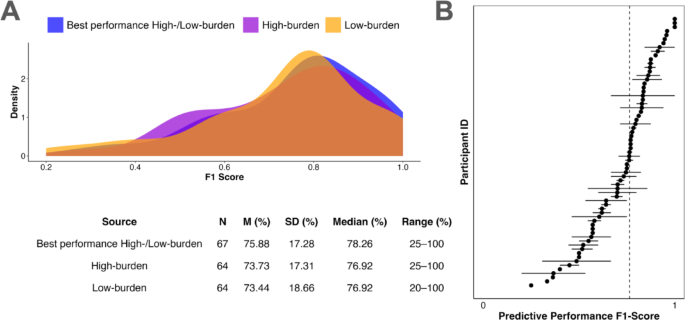
Beck, E. D. & Jackson, J. J. Personalized prediction of behaviors and experiences: an idiographic Person–Situation test. Psychol. Sci. 33, 1767–1782 (2022).
Google Scholar
Jovanova, M. A person-specific Approach To Predict Health Behaviors: a Proof of Concept (University of Pennsylvania, 2023).
Guizar-Heredia, R. et al. A new approach to personalized nutrition: postprandial glycemic response and its relationship to gut microbiota. Arch. Med. Res. 54, 176–188 (2023).
Google Scholar
Heber, D., Li, Z. & Ordovas, J. Precision Nutrition: the Science and Promise of Personalized Nutrition and Health (Elsevier, 2023).
Ceriello, A. Postprandial hyperglycemia and diabetes complications: is it time to treat? Diabetes 54, 1–7 (2005).
Google Scholar
Liu, J. et al. Projected rapid growth in diabetes disease burden and economic burden in china: a spatio-temporal study from 2020 to 2030. Lancet Reg. Health West. Pac. 33, 100700 (2023).
Google Scholar
Model of personalized postprandial. Glycemic response to food developed for an Israeli cohort predicts responses in Midwestern American individuals. Am. J. Clin. Nutr. 110, 63–75 (2019).
Google Scholar
Berry, S. E. et al. Human postprandial responses to food and potential for precision nutrition. Nature Medicine 26, 964–973 (2020).
Søndertoft, N. B. et al. The intestinal Microbiome is a co-determinant of the postprandial plasma glucose response. PLOS ONE. 15, e0238648 (2020).
Google Scholar
The physiologic. And phenotypic significance of variation in human amylase gene copy number. Am. J. Clin. Nutr. 108, 737–748 (2018).
Google Scholar
Dods, R. F. Understanding Diabetes: A Biochemical Perspective (Wiley, 2013).
Rayner, C. K., Samsom, M., Jones, K. L. & Horowitz, M. Relationships of upper Gastrointestinal motor and sensory function with glycemic control. Diabetes Care. 24, 371–381 (2001).
Google Scholar
Marathe, C. S. et al. Hypoglycaemia and gastric emptying. Diabetes Obes. Metabolism. 21, 491–498 (2019).
Google Scholar
Horowitz, M., Edelbroek, M. A., Wishart, J. M. & Straathof, J. W. Relationship between oral glucose tolerance and gastric emptying in normal healthy subjects. Diabetologia 36, 857–862 (1993).
Google Scholar
Shukla, A. P., Iliescu, R. G., Thomas, C. E. & Aronne, L. J. Food order has a significant impact on postprandial glucose and insulin levels. Diabetes Care. 38, e98–e99 (2015).
Google Scholar
Ferguson, B. K. & Wilson, P. B. Ordered eating and its effects on various postprandial health markers: A systematic review. J. Am. Nutr. Assoc. 42, 746–757 (2023).
Google Scholar
Acute effect of. Late evening meal on diurnal variation of blood glucose and energy metabolism. Obes. Res. Clin. Pract. 5, e220–e228 (2011).
Google Scholar
Stevens, S. et al. The effectiveness of digital health technologies for patients with diabetes mellitus: A systematic review. Front. Clin. Diabetes Healthc. 3, 936752 (2022).
Google Scholar
Doyle-Delgado, K. & Chamberlain, J. J. Use of diabetes-Related applications and digital health tools by people with diabetes and their health care providers. Clin. Diabetes. 38, 449–461 (2020).
Google Scholar
Lehmann, M., Jones, L. & Schirmann, F. App engagement as a predictor of weight loss in Blended-Care interventions: retrospective observational study using Large-Scale Real-World data. J. Med. Internet. Res. 26, e45469 (2024).
Google Scholar
Debong, F., Mayer, H. & Kober, J. Real-World assessments of mysugr mobile health app. Diabetes Technol. Ther. 21, S235–S240 (2019).
Google Scholar
Sherazi, A. B. et al. Functions of mHealth diabetes apps that enable the provision of pharmaceutical care: criteria development and evaluation of popular apps. Int J. Environ. Res. Public. Health 20, 64 (2022).
Jovanova, M. et al. Psychological distance intervention reminders reduce alcohol consumption frequency in daily life. Sci. Rep. 13, 1–14 (2023).
Google Scholar
Engeroff, T., Groneberg, D. A. & Wilke, J. After dinner rest a while, after supper walk a mile?? A systematic review with Meta-analysis on the acute postprandial glycemic response to exercise before and after meal ingestion in healthy subjects and patients with impaired glucose tolerance. Sports Med. 53, 849–869 (2023).
Google Scholar
Kaur, B., Koh, M., Ponnalagu, S. & Henry, C. J. Postprandial blood glucose response: does the glycaemic index (GI) value matter even in the low GI range? Nutr. Diabetes. 10, 1–8 (2020).
Google Scholar
Roshan, S. et al. The PROVIDE study: primary care assessment of the ROche IPDM tools for validation and implementation in diabetes management and evaluation. MedRxiv 2023.12.23.23300283 (2023).
Crossen, S. S., Romero, C. C., Lewis, C. & Glaser, N. S. Remote glucose monitoring is feasible for patients and providers using a commercially available population health platform. Front. Endocrinol. 14, 1063290 (2023).
Google Scholar
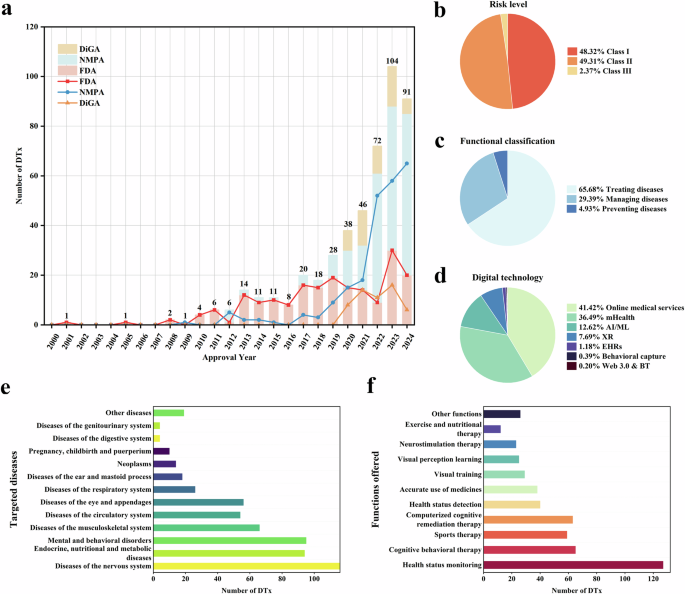
Giger, O. F. et al. Digital health technologies and innovation patterns in diabetes ecosystems. Digit. HEALTH. (2025).
Google Scholar
Gastaldi, G. et al. Swiss recommendations of the society for endocrinology and diabetes (SGED/SSED) for the treatment of type 2 diabetes mellitus (2023). Swiss Med. Wkly. 153, 40060 (2023).
Google Scholar
Giger, O. F., Fleisch, E., Jovanova, M. & Kowatsch, T. Barriers and facilitators of implementing value-based care: the case of SwissDiabeter. Digit. Health. 11, 20552076251336322 (2025).
Google Scholar
Wolffenbuttel, B. H. R. et al. Ethnic differences in glycemic markers in patients with type 2 diabetes. Diabetes Care. 36, 2931–2936 (2013).
Google Scholar
Kodama, K. et al. Ethnic differences in the relationship between insulin sensitivity and insulin response: A systematic review and meta-analysis. Diabetes Care. 36, 1789–1796 (2013).
Google Scholar
Rajput, D., Wang, W. J. & Chen, C. C. Evaluation of a decided sample size in machine learning applications. BMC Bioinform. 24, 1–17 (2023).
Google Scholar
Brügger, V., Kowatsch, T. & Jovanova, M. Wearables and smartphones for modifiable risk factors in metabolic health: a scoping review protocol. BioRxiv (2024).
Google Scholar
Walton, A., Nahum-Shani, I., Crosby, L., Klasnja, P. & Murphy, S. Optimizing digital integrated care via Micro-Randomized trials. Clin. Pharmacol. Ther. 104, 53–58 (2018).
Google Scholar
Fuchs, M., Wirth, B., Bilz, S., Brändle, M., Kowatsch, T. & Jovanova, M. Exploring message receptivity and protocol adherence in a clinical study: a micro-randomized trial protocol. Proc. CHI Conf. Hum. Factors Comput. Syst. 2025, Yokohama, Japan (2025).
Relationship between. intra-individual variability in nutrition-related lifestyle behaviors and blood glucose outcomes under free-living conditions in adults without type 2 diabetes. Diabetes Res. Clin. Pract. 196, 110231 (2023).
Google Scholar
Rao, W. & Diabetes Datasets ShanghaiT1DM and ShanghaiT2DM. (2023). https://doi.org/10.6084/m9.figshare.c.6310860
Gabir, M. M. et al. The 1997 American diabetes association and 1999 world health organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care. 23, 1108–1112 (2000).
Google Scholar
Nguyen, A. & White, J. R. FreeStyle libre 3. Clin. Diabetes. 41, 127–128 (2022).
Google Scholar
Zheng, Y. et al. A community-based cross-sectional study of dietary composition and associated factors among tuberculosis patients in China. Sci. Rep. 14, 2676 (2024).
Google Scholar
Jacober, S. J. et al. Basal insulin peglispro: overview of a novel long-acting insulin with reduced peripheral effect resulting in a hepato-preferential action. Diabetes Obes. Metab. 18 (Suppl 2), 3–16 (2016).
Google Scholar
NHS. About intermediate-acting insulin. (2023). https://www.nhs.uk/medicines/insulin/intermediate-acting-insulin/about-intermediate-acting-insulin/
Howard, J. Y. & Watts, S. A. Bolus insulin prescribing recommendations for patients with type 2 diabetes mellitus. Fed. Pract. 34, S26–S31 (2017).
Google Scholar
Arungarinathan, G., McKay, G. A. & Fisher, M. Drugs for diabetes: part 4 acarbose. Br. J. Cardiol. 18 (2), 78–81 (2011).
Brouns, F. et al. Glycaemic index methodology. Nutr. Res. Rev. 18, 145–171 (2005).
Google Scholar
Li, Q., Bedi, T., Lehmann, C. U., Xiao, G. & Xie, Y. Evaluating short-term forecasting of COVID-19 cases among different epidemiological models under a Bayesian framework. Gigascience 10, (2021).
Vabalas, A., Gowen, E., Poliakoff, E. & Casson, A. J. Machine learning algorithm validation with a limited sample size. PLOS ONE. 14, e0224365 (2019).
Google Scholar
The effect of. Machine learning regression algorithms and sample size on individualized behavioral prediction with functional connectivity features. NeuroImage 178, 622–637 (2018).
Google Scholar
Dhiman, P. et al. Sample size requirements are not being considered in studies developing prediction models for binary outcomes: a systematic review. BMC Med. Res. Methodol. 23, 1–11 (2023).
Google Scholar
Soyster, P. D., Ashlock, L. & Fisher, A. J. Pooled and person-specific machine learning models for predicting future alcohol consumption, craving, and wanting to drink: A demonstration of parallel utility. Psychol. Addict. Behav. 36, 296–306 (2022).
Google Scholar
Jacobson, N. C. & Chung, Y. J. Passive sensing of prediction of Moment-To-Moment depressed mood among undergraduates with clinical levels of depression sample using smartphones. Sensors (Basel) 20, 3572 (2020).
Chen, T. & Guestrin, C. XGBoost. in Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data MiningACM, New York, NY, USA, (2016). https://doi.org/10.1145/2939672.2939785
Zignoli, A., Skroce, K., Lipman, D. J. & Zisser, H. C. Personalized nutrition and machine-learning: exploring the scope of continuous glucose monitoring in healthy individuals in uncontrolled settings. Biomed. Signal. Process. Control. 90, 105809 (2024).
Google Scholar
Agah, A. Medical Applications of Artificial Intelligence (CRC, 2013).
Prendin, F. et al. The importance of interpreting machine learning models for blood glucose prediction in diabetes: an analysis using SHAP. Sci. Rep. 13, 16865 (2023).
Google Scholar
link