Impact of a novel smartphone application for remote monitoring of gestational diabetes on glycaemic control and birth outcomes: a pilot observational study
During the study period (January–December 2021) 483 positive oral glucose tolerance tests were reported by the public obstetric diabetes service at the Rotunda hospital. This tertiary level university teaching hospital cared for 10,715 pregnant mothers and delivered 9147 babies in 2021 with an 8.4% incidence of new-GDM diagnosis among antenatal patients. Patients in the app-assisted pathway of care were representative of the GDM population at our hospital for ethnicity, BMI, parity, and age. Table 1 demonstrates the baseline characteristics and demographic information of women in the app-assisted care group and of a historical cohort of women with GDM. Patients were recruited and consented to both standard approach to GDM care in addition to use of ‘GDMapp’. Demographic and outcome data for this app-assisted care group were compared to a similar group of GDM patients attending the obstetric diabetes service at the Rotunda Hospital in the time period directly antecedent to commencement of recruitment to app-based care.
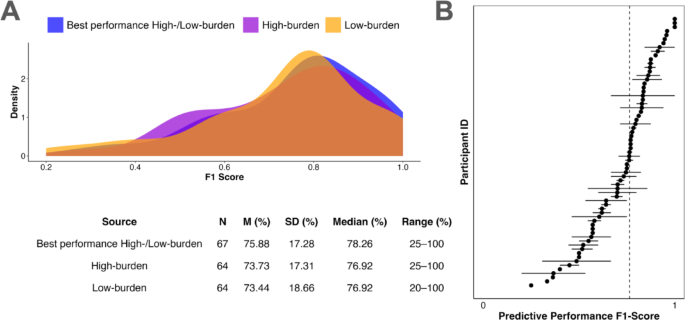
There were 77 patients during a two-month period of the study when the hospital systems were impacted by the after-effects of a malware attack on its IT services, where pre-screening was not possible in advance of their hospital visit. These patients were considered to have been missed. Of the remaining eligible patients, 169 (55.7%) consented to participate in this study. Figure 1a–c represents a flow diagram of recruitment to the study.
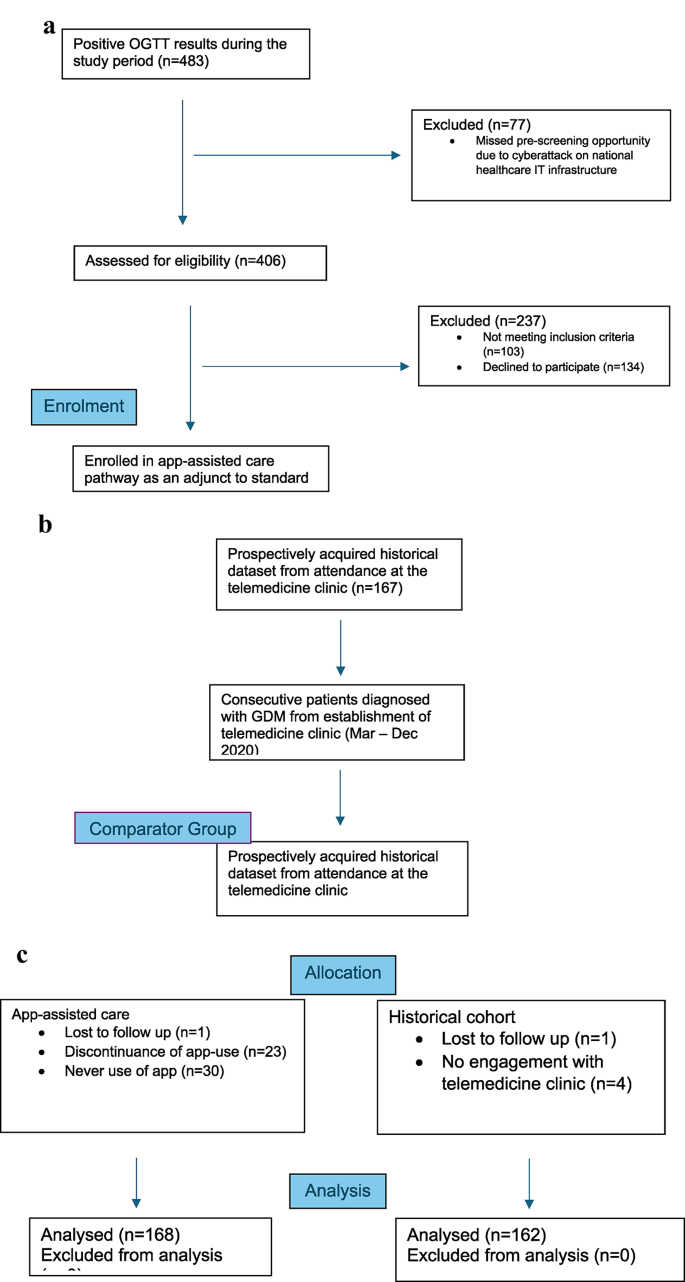
a Pathway to enrolment in app-assisted care arm. b Pathway to enrolment in historical cohort arm. c Pathway to allocation and analysis.
Glycaemic control
Despite the standardised approach to management through the telemedicine clinic, participants engaged in app-assisted care for GDM had a greater number of recorded glycaemic indices across both fasting and postprandial assessments, available for review by the obstetric diabetes team.
Further interrogation of the glycaemic results demonstrated a 2-point difference in the mean fasting results from 5.0 mmol/l in the historical group to 4.8mmol/l in the app-assisted group (Table 2). This finding was further buttressed by a 5-point reduction in mean postprandial glycaemic indices (p < 0.001). The standard deviation for both the mean fasting and mean postprandial levels in the app-assisted care group indicate a high degree of concentration of the overall values around their respective means. Achievement of good glycaemic control was demonstrated in both groups, but the app-assisted group demonstrated superior optimisation of that control across both fasting and postprandial assessments.
This study demonstrates the achievability of maintaining fasting glycaemic indices below the set threshold of 5.3 mmol/l on more than 70% of occasions with the use of app-based care (Figs. 2 and 3). Similarly, the 90th percentile for postprandial indices was 7.3 mmol/L, aligning well with the commonly adopted postprandial target threshold of 7.8 mmol/L which was chosen as a cut-off in this analysis9. An achievement of optimised postprandial blood glucose levels by 98.2% (n = 165) was noted in the app-assisted care group. While the postprandial data were excellent in the historical control group (96.3%, n = 162), further analysis identified that fewer patients with above-threshold postprandial readings at any time point in the app-using group (33.3%) subsequently required pharmacological intervention compared with patients reporting above threshold postprandial indices in the historical control group (83.3%).
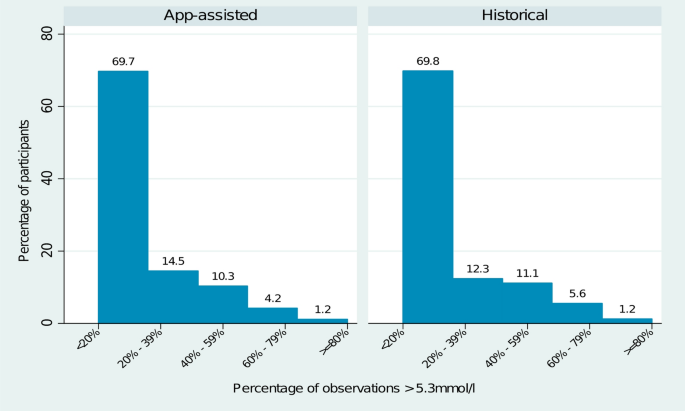
Percentage of observations per participant across both groups greater than 5.3 mmol/l fasting threshold.
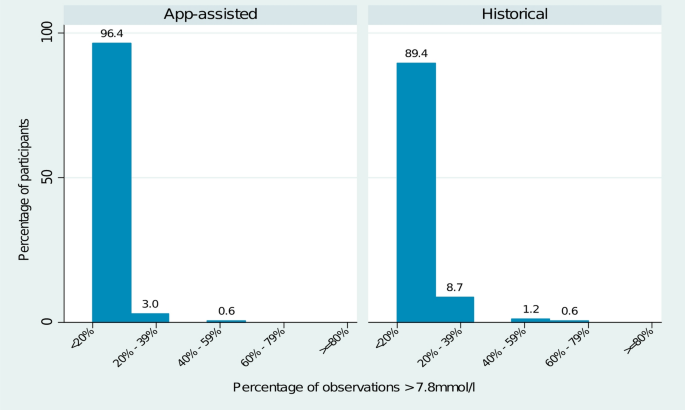
Percentage of observations per participant across both groups greater than 7.8 mmol/l postprandial threshold.
Requirement for supplemental hypoglycaemic therapy
Decisions regarding initiation of treatment were made by the same physician for patients in both groups, reducing the impact of bias. A greater proportion of patients in the historical cohort (15.4%, n = 25) were commenced on supplemental therapy of any description compared with the app-assisted group (8.92%, n = 15) however this did not quite reach statistical significance (p = 0.064). The mean number of weeks prior to requirement for and initiation of pharmacological treatment was greater in the app-assisted care group, and this did reach statistical significance (p = 0.008). Supplemental therapy (metformin or insulin or both) was initiated at a mean gestational age of 33 weeks 3 days and 31 weeks 6 days for the app-assisted and historical cohorts respectively. For both groups, treatment was initiated when > 30% of blood glucose values in a set time-period exceeded the agreed-upon thresholds (fasting > 5.3 mmol/L and postprandial > 7.8 mmol/L).
Delivery and birth outcomes
Outcome data relating to labour, delivery and birth are presented in Table 3. The mean gestational age at delivery in the intervention (app-using) group was 38 + 3 and that for the historical control group was 39 + 3. Similar rates of induction of labour in both groups were observed (47.3% versus 46.9%) (p-value 0.999). The overall rate of caesarean delivery was higher in the historical control group (41.8%) compared with 32.7% in the app-using group. While the incidence of delivery by emergency caesarean section was similar in both groups (55% vs. 64%, p = 0.142), there were fewer elective caesarean sections (n = 25, 15%) in the app-using group but a higher rate of operative vaginal deliveries (n = 34, 20.4%).
Maternal and neonatal outcomes
The individual instances relating to complications and adverse maternal outcomes were low across both groups investigated for this study and, as such, a composite maternal outcome of pre-eclampsia, pregnancy induced hypertension, preterm prelabour rupture of membranes and postnatal readmission rather than individual variables were considered (Table 3).
The mean birthweight was 115.4 g less among the app-assisted care group than the historical cohort (p-value 0.080). Reflecting the difference in the mean birthweights, the mean birthweight centiles were 51.216 (2.5–97.5) and 53.41 (2.5–97.5) in the app-cohort and historical cohort respectively (p-value 0.348). Macrosomia, defined as birthweight > 4000 g, was identified in 13.6% (n = 23) of app-assisted care cases and in 17.9% (n = 29) of the historical comparator group (p = 0.127).
The incidence of shoulder dystocia was low in each group and as such was considered as part of a composite measure of ‘birth complications’.
Admission rates to the neonatal intensive care unit (NICU) were similar across both groups (15.6%, n = 26; 16.1%, n = 26). The most common indication for admission to the NICU in the app-using group was for transient respiratory support. Jaundice surveillance and phototherapy represented the most common reason for NICU admission in the historical group. Incidence of neonatal jaundice and mean neonatal bilirubin levels did not reach statistical significance when comparisons between the two groups were made.
Service utilisation
The mean number of encounters in the app-assisted care group, for the purposes of GDM management alone, was 4.14 (SD 1.46) while that for the historical control group was 4.61 (SD 4.13), a finding that reached statistical significance (p < 0.012). Within the app-assisted care group there were 19.2% fewer participants who required additional dietetics review beyond the usual input from the dietician at the time of initial diagnosis with this again reaching statistical significance (p < 0.001).
Equal percentages of participants requiring supplemental dietetics guidance in both groups had above threshold glucose readings > 30% of occasions (41.3%, n = 24; 41.3%, n = 36).
App-using participants had a statistically significant shorter length of postnatal hospital stay compared to those in the historical cohort (p < 0.0045).
Stakeholder satisfaction
Both patient app-users and staff in the obstetric diabetes service were asked to complete specifically formulated questionnaires assessing app reliability, functionality and acceptability. The app and hospital portal scored high satisfaction rates across all three of these domains for both groups.
link